
Source: International Stem Cell Research
According to a report in Medicine, the West China Hospital used mesenchymal stem cells to treat a case of Behcet's disease with recurrent leg ulcers that had failed to respond to conventional treatment. This is also another remarkable achievement of stem cell therapy in lower limb ulcers after diabetic foot.
What is venous leg ulcer?
The more common type of chronic ulcer of the lower extremities is venous leg ulcer (VLU), which accounts for about 80%.
venous leg ulcer (VLU) is an open skin lesion that occurs in the legs or feet. Local skin lesions can be seen erosion, defects, often accompanied by pus or scab, after healing may leave scars. And ulcer wounds are prone to repeated attacks, prolonged and not healed, increasing the risk of infection at the same time, will also aggravate the pain of patients, seriously affect the quality of life, but also to the family has brought a heavy economic burden and nursing pressure.
The main cause of VLU is blood stasis in calf veins caused by various factors (such as venous valve insufficiency, post-deep vein thrombosis syndrome, etc.), which leads to venous hypertension and thus causes disease. In addition, advanced age (age >55 years), trauma, obesity, sedentary lack of exercise, and lower limb bone and joint diseases may also increase the risk.
Remarkable results of stem cell therapy for lower limb ulcers
Behcet's disease was associated with recurrent leg ulcers. After treatment with mesenchymal stem cells, the ulcers were relieved and the function of the affected leg returned to normal
Behcet's disease (BD) is a systemic, vascular inflammatory disease characterized by oral and genital mucosal ulcers, uveitis, retinal vasculitis, and skin lesions. For BD patients with complex and destructive leg ulcers, there is no effective clinical treatment.
The patient is a 55-year-old woman who has had the disease for 8 years. The main symptoms at present are generalized nodular erythematoid papular impetigo lesions, recurrent oral and genital ulcers, recurrent leg ulcers, and difficulty walking. Conventional immunosuppressive therapy and anti-tumor necrosis factor inhibitors (etanercept, adamyumab) have not shown significant effects. Mesenchymal stem cells (MSC) combined with low-dose immunosuppression (prednisone + thalidomide) were administered.
Follow-up showed that after 2 months of mesenchymal stem cell treatment, the ulcer of the patient's right leg improved significantly, and the ulcer of the left leg healed completely. After 3 months of treatment, the symptoms of Behcet's disease (oral and genital ulcers, papular impetigo lesions) improved significantly. During a follow-up period of up to 34 months, the ulcer lesions remained in remission, the affected leg function was normal, and no significant side effects were observed.
These results suggest that mesenchymal stem cell therapy may be a potential treatment for refractory, drug-resistant Behcet patients with leg ulcers.
The closure rate of diabetic foot ulcer was over 75% after SVF cell therapy
Diabetic foot ulcer is the result of diabetes-induced microarteriolar vascular disease and peripheral neuropathy, which can involve skin, blood vessels, nerves, tendons, bones, etc., and its disease is easy to relapse, and often complicated with infection, which has been a difficult problem in clinical treatment. In recent years, stem cells and their derivatives have achieved remarkable results in the treatment of diabetic foot, providing a new treatment strategy for patients.
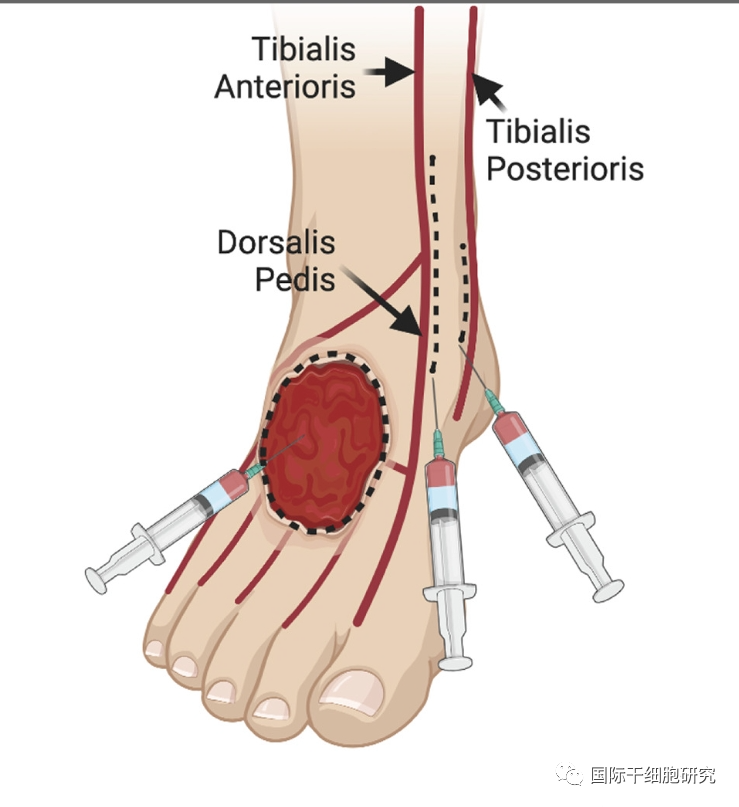
The journal Stem Cell Translational Medicine published an article on "A Phase I clinical study of autologous adipose-derived stromal vascular component (SVF) cells for the treatment of diabetic foot ulcers." The study included 63 patients with type 2 diabetes with chronic diabetic foot ulcers (ulcer surface diameter > 3cm). After treatment begins, SVF cells are injected into and around the ulcer bed by local injection.
After follow-up, at 6 months of treatment, 51 patients had a diabetic foot ulcer closure rate of 100% and 8 subjects had a closure rate of ≥75%. At 12 months of treatment, the ulcer cure rate was 100% in 50 subjects and ≥85% in 4 subjects. The Doppler study of 11 subjects showed an increase in peak systolic velocity and pulse index in 33 of the 33 arteries, consistent with an increase in distal artery outflow.
The results show that SVF can be used to treat chronic diabetic foot ulcers, with evidence of wound healing, vascular repair and generation. However, in Asia, umbilical cord mesenchymal stem cells and Japanese autologous fat stem cells are widely used in the treatment of diabetic foot ulcers.
Why can stem cells treat leg venous ulcer wound?

Skin wound healing is a continuous and complex process that is essential for maintaining the barrier function of the skin and usually involves three stages: inflammation, cell proliferation and migration, and tissue remodeling. Recent studies have found that stem cells with the ability of self-renewal and multidirectional differentiation can accelerate wound healing by acting on multiple aspects of wound healing, mainly due to the following aspects:
1、Promote angiogenesis
Rich blood supply can provide nutrition for wound healing, and rich vascular network plays an important role in absorbing necrotic materials and alleviating local wound infection.
Studies have shown that autologous fat stem cells can contribute to the formation of new blood vessels and promote wound healing by secreting a variety of cytokines closely related to angiogenesis, such as IL-6 (interleukin-6), VEGF (vascular endothelial growth factor), and TGF-β (transforming growth factor-β).
2、Promote epithelialization
Epithelialization is an important sign of wound healing, and only complete epithelialization of the wound can prevent water loss and resist pathogen infection. However, patients with venous leg ulcers are often infected (such as staphylococcus aureus, streptococcus), which leads to delayed wound healing.
Studies have shown that after stem cell therapy, the expression of fibronectin in wound tissue is increased, and the proliferation of dermal and epidermal cells is enhanced, thus promoting the formation of wound epithelium and ultimately contributing to the healing of ulcer surface.
3、Regulate extracellular matrix (ECM) synthesis
ECM plays a "skeletal" role in wound healing. In the process of wound repair, ECM composed of type I collagen forms a scar that temporarily closes the wound to accelerate scar formation and shorten the healing time of the wound.
Studies have shown that Japanese autologous fat stem cells can regulate the remodeling process of ECM. In the course of treatment, such stem cells accelerate the remodeling of ECM in the process of wound repair by up-regulating the ratio of type III collagen to type I collagen, thus promoting the healing of ulcer surface.
4、Regulate macrophages
If the wound is always in the inflammatory response stage, it is difficult to heal, and macrophages can play an important role in the inflammatory response.
Studies have shown that stem cells can regulate the aggregation, number and type of macrophages by secreting various cytokines, such as TNF and IL-10, and ultimately regulate macrophages to promote wound healing.
5、Modulating cellular immunity
After the inflammatory period, the immune response gradually weakens without negative feedback, resulting in the continued abnormal presence of immune cells, which affects the rate of tissue healing.
Research has shown that stem cells can reduce inflammation, regulate cellular immunity, and promote wound healing through direct cell contact and secretion of cytokines.
Small series message
The treatment of venous ulcers of lower limbs is difficult. Compared with traditional methods such as surgery, drugs, local wound treatment and pressure treatment, stem cell therapy has unique advantages, which can help accelerate wound healing, improve treatment effect and patients' quality of life. At present, there are more than 50 clinical trials of MSCs refractory wounds of lower limbs registered in the United States clinical trials, including venous ulcer (3) and diabetic foot (23). Xiaobian also hopes that with the continuous deepening of stem cell research, the traditional treatment model can be broken in the future, and new hope will be brought to patients with relapse or refractory disease!