
As one of the major breakthroughs in the field of stem cells, organoid technology has attracted much attention in the field of medical research, and the technology has developed rapidly in the short decade since the advent of the technology, and relevant papers have exploded, and it is even predicted to be the next Nobel Prize.
Organoids are clusters of cells formed by three-dimensional culture in vitro using stem cells and contain some key properties of the organ they represent. Although organoids are not human organs in the real sense, they can simulate real organs in structure and function, and can simulate the structure and function of tissues in the body to the greatest extent, and can be long-term stable subculture.
Stem cells have the potential of multidirectional differentiation and self-renewal, and can be directed into a variety of human cells, including cardiomyocytes, osteoblasts, nerve cells, and so on, under certain circumstances, and are ideal sources for the cultivation of Organoids.
Fetal brain tissue produces 3D "mini" organoids
Scientists never stop exploring the development of the human brain. For the first time, a team of researchers from the Princess Maxima Pediatric Oncology Center and the Hubrecht Institute, led by Hans Clevers, a pioneer in the field of organoids, has successfully derived a self-organizing brain organoid (FeBO) from human fetal brain tissue. The relevant research results were published in the top academic journal "Cell" (impact factor IF =64.5), which achieved a "milestone" in the development of organoid technology in the field of brain research, and opened up a new path for in-depth research on brain development, and exploration of brain development disorders, brain tumors and other brain development related diseases.
Previously, brain organoids were grown in the lab. Now, scientists have developed brain organoids directly from human fetal brain tissue. New research has found that using small pieces of fetal brain tissue, rather than individual cells, is crucial to creating a "mini" brain. These small pieces of fetal brain tissue can self-organize into organisms.
The origin and development of organoids
As early as the 1980s, the term "organoid" was coined.
In 2009, Hans Clevers' team at the Hubrecht Institute in the Netherlands successfully cultured Lgr5+ intestinal stem cells in vitro into small-intestinal organoids with the crypts and villi structures of the small intestine.
In 2013, researchers from Japan, Germany, and the United States built liver buds, mini-kidneys, and mini-brains, respectively, making the field gain widespread international attention. In the same year, organoids were named the top 10 technologies of the year by Science.
In early 2018, organoids were named the best Technology of 2017 by Nature Method, and the evaluation was given: The use of stem cells to directly induce the generation of three-dimensional tissue models provides a powerful method for human biological research.
In 2019, the world's three top journals CNS(CELL "Cell", Nature "Nature", Science "Science") launched a special issue on organoid technology.
At present, stem cells have successfully constructed a variety of organ organoids with some key physiological structures and functions, including retina, small intestine, stomach, brain, liver, pancreas, kidney, heart, etc. There are not only normal organ tissue organoids, but also corresponding tumor tissue organoids.
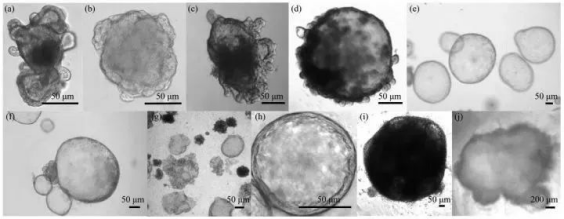
Topography of different organoids
(a) Small intestine organoids.(b) Colon organoids.(c) Esophagus organoids.(d) Stomach organoids.(e) Liver organoids.(f) Pancreas organoids.(g) Lung organoids.(h) Breast organoids.(i) Kidney organoids.(j) brain organoids
The world's first organoid transplant was successfully carried out
As early as July 2022, a research team at Tokyo Medical and Dental University in Japan announced the implementation of a clinical study of stem cell-derived organoids for human transplantation, and they transplanted an organoid cultured with the patient's own healthy intestinal mucosal stem cells in a patient with refractory ulcerative colitis.
This attempt at regenerative medicine is the first of its kind in the world, and the safety of this trial of stem cell-derived organoids will be verified within the next year.
The research team used an endoscope to collect normal large intestine mucosa (containing many cells such as stem cells) from patients, and cultured it for about a month to build "organoids" with a diameter of 0.1 to 0.2 millimeters.
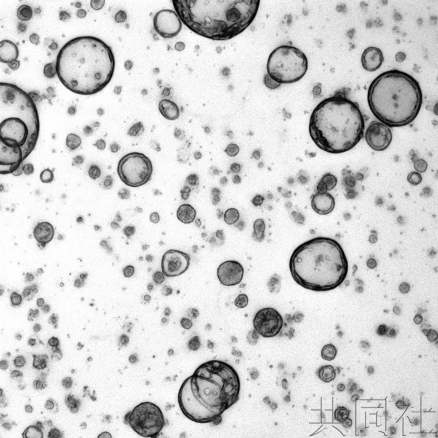
Microscope photo of cell blocks made by the Kyodo/Tokyo Medical and Dental University team using cultures of large intestine mucosa
The researchers then transplanted the "organoids" into the patient's large intestine, covered them with a film that degrades inside the body, and tried to repair the damaged mucosa with the patient's own tissue. The procedure does not require open surgery. It is reported that the "organoid" transplant was carried out on July 5 and the patient is currently in good condition.
In the next year and a half, the research team plans to transplant seven patients who are unable to respond to existing drugs, and to further confirm the effectiveness and safety of this emerging technology. If it goes well, it not only means that ulcerative colitis may be completely cured, but also is expected to promote the treatment of "Crohn's disease", a refractory disease that mainly occurs in the digestive tract with chronic inflammation.
Sum up
As a cutting-edge technology that has been officially born for only ten years, the wide application of stem cell derived organoid technology is still in its infancy, but it has shown the potential to treat intractable diseases. It is believed that with the deepening of stem cell and organoid research and the continuous maturity of technology, stem cell derived organoids will play an increasingly important role in translational medicine and clinical personalized therapy.