
Stem cell research is developing rapidly, offering exciting possibilities for treating a variety of diseases and injuries. Two outstanding figures in this field are: mesenchymal stem cells (MSC) and induced pluripotent stem cells (iPSC). Although both have great promise, their origins, characteristics and potential applications vary. Let's explore these fascinating cell types and see how they can contribute to the future of regenerative medicine.
It is important to understand the ethical considerations of stem cell research. Research has traditionally relied on embryonic stem cells (ESCs), which has raised ethical concerns about embryo destruction. MSC and iPSC provide alternative solutions that bypass these concerns.
Mesenchymal stem cells (MSC):
MSCs are derived from various adult tissues, such as bone marrow, adipose tissue and umbilical cord, and have attracted much attention due to their regenerative properties and immunoregulatory effects. MSCs can differentiate into osteoblasts, chondrocytes and adipocytes, and have broad application prospects in tissue repair and inflammation regulation.
Main attributes of MSCs:
1. Tissue repair:
Pluripotent differentiation: Although MSCs are not pluripotent, they are pluripotent, allowing them to differentiate into a specific set of specialized cell types within a specific lineage. For example, bone marrow-derived MSCs can differentiate into osteoblasts (osteocytes), chondrocytes (chondrocytes), and adipocytes (adipocytes). This targeted ability to differentiate allows MSCs to directly participate in tissue repair.
Paracrine coordination: In addition to direct cell replacement, MSCs also exert a powerful influence through paracrine effects. They secrete a complex mixture of growth factors, cytokines and other signaling molecules. This combination of molecules creates a supportive microenvironment that stimulates the body's intrinsic healing mechanisms. These factors promote cell proliferation, migration and differentiation of resident stem cells, ultimately promoting tissue regeneration.
2. Immunomodulation:
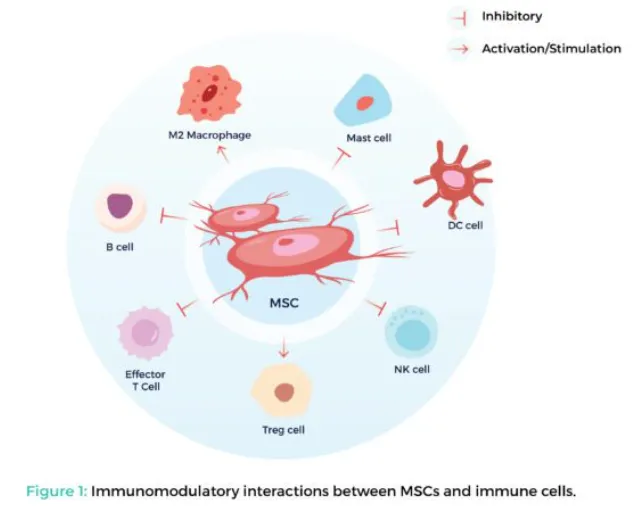
Master of Immune Balance: MSCs have significant immunoregulatory properties. They can interact with and affect the activity of various immune cells, including T cells, macrophages, and natural killer cells. This effect promotes an anti-inflammatory response, which is critical to alleviating the harmful effects of an overactive immune system. This makes MSCs potential candidates for treating autoimmune diseases (the body attacks its own tissue) and graft-versus-host disease (GVHD)(a life-threatening complication after bone marrow transplantation).
Mechanism of immune regulation: The exact mechanism by which MSC regulates the immune system is still under study. However, some key approaches include:
Inhibiting the proliferation of pro-inflammatory T cells
Induction of regulatory T cells (Treg) that promote immune tolerance
Decreases the activity of antigen presenting cells, which play a key role in activating the immune response
3. Risk of oncogenesis is minimal:
Limited self-renewal ability: Compared to pluripotent stem cells, MSC has limited self-renewal ability. This means that a cell divides a limited number of times, after which the cell stops proliferating. This limited ability to self-renew significantly reduces the risk of uncontrolled cell growth and tumor formation after transplantation.
Strict safety protocols: Despite the low risk, researchers put safety first. Strict quality control measures and extensive preclinical testing are critical to ensuring the safe and effective application of MSC therapy.
Induced pluripotent stem cells (iPSC):
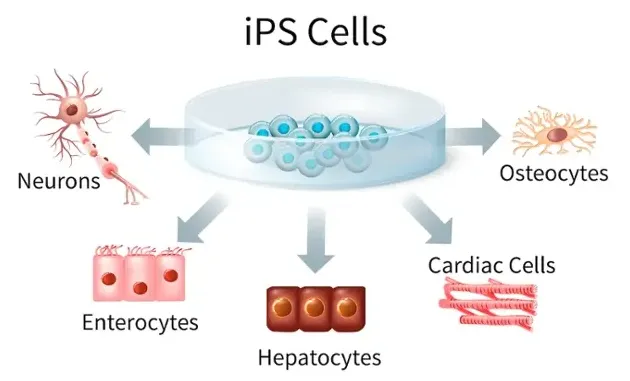
iPSC is produced by cellular reprogramming of adult somatic cells and is attractive for pluripotency and patient-specific. Although still in early stages of development, iPSC can differentiate into almost any cell type in the body, providing unparalleled opportunities for treatment, disease models, drug development and personalized medicine.
Key attributes of iPSC:
1. Plurality:
Cellular chameleon: Unlike MSCs, iPSC has extraordinary pluripotency. This means they have the potential to differentiate into any cell type found in adults-muscle cells, neurons, skin cells, germ cells, and so on. This reflects the development potential of embryonic stem cells (ESCs), but avoids the ethical issues surrounding their use.
Release therapy possibilities: The pluripotency of iPSC allows scientists to generate specific cell types associated with a variety of diseases. For example, iPSC from patients with neurological disorders can differentiate into neurons with the same genetic mutations. This opens the door to studying disease mechanisms and developing targeted therapies.
2. Disease modeling:
Patient-specific cell models: The ability to generate iPSCs from patients 'own cells is a major change in disease modeling. These patient-derived iPSCs can differentiate into specific cell types affected by the disease, creating personalized cell models. The model allows researchers to study disease processes in a controlled laboratory environment, mimicking the unique genetic makeup of patients.
Uncovering disease mechanisms: By studying patient-derived iPSC models, researchers can gain insight into the molecular and cellular mechanisms behind various diseases. This knowledge can help identify new treatment targets and develop more effective treatment strategies.
3. Personalized treatment
Minimize immune rejection: A significant advantage of iPSC is its ability to be used for personalized cell therapies. Because these cells originate from the patient's own tissue, they are much less likely to be rejected by the immune system, eliminating a major obstacle to traditional cell therapy.
The future of regenerative medicine: Personalized cell therapy using patient-derived iPSC holds promise to treat a variety of diseases. These therapies may involve transplanting healthy, labor-cultured cells from a patient's iPSC to replace damaged or diseased cells. This approach has the potential to treat diseases such as Parkinson's disease, heart failure and certain genetic diseases.
The future of stem cell therapy:
MSC and iPSC are not competitors, but complementary tools with different advantages. As research progresses, we can look forward to seeing these cell types play an increasingly important role in regenerative medicine. By leveraging their potential, scientists can develop innovative therapies and potentially cure multiple diseases.