
According to the official website of the "Australia Government Department of Health and Elderly Care", the Australia government will invest US$55.24 million in the research and development of stem cell therapy and infrastructure construction, mainly through the development of new treatment methods to alleviate refractory diseases such as osteoarthritis and rheumatoid arthritis.
Osteoarthritis and rheumatoid arthritis have always been a long-standing problem in bone and joint diseases. Patients may suffer from joint pain and deformity, which seriously affects daily life. In recent years, with the emergence of regenerative therapies such as stem cells, it has brought new dawn to such patients!
Osteoarthritis and Rheumatoid Science
Osteoarthritis

"Osteoarthritis (OA)", also known as "senile arthritis" and "degenerative arthritis", is a chronic joint degenerative disease characterized by secondary bone hyperplasia and degenerative changes in articular cartilage. It can occur in many joints in the body, of which the knee joint is the most common.
Knee osteoarthritis (KOA) is one of the most common types of osteoarthritis (OA). The main feature is damage to cartilage and subchondral bone. Patients may experience joint pain, stiffness, limited movement, and joint deformity. Intraarticular injection of mesenchymal stem cells (MSC) with immunoregulatory properties provides a non-invasive treatment for patients with osteoarthritis that helps relieve pain and promotes cartilage regeneration.
Rheumatoid arthritis

Rheumatoid arthritis (RA) is a chronic inflammatory autoimmune disease. Common symptoms include joint pain, joint swelling, joint stiffness, etc., which is often followed by joint dysfunction, and in severe cases, it can even lead to progressive disability.
At present, there is no good treatment method. Clinically, symptomatic treatment such as corticosteroids and anti-rheumatic drugs is the main treatment. However, long-term use of anti-rheumatic drugs may lead to drug resistance in patients, resulting in poor treatment effects.
Mesenchymal stem cells can differentiate into various tissues such as cartilage, muscle, tendon, ligament, and bone, and can regulate immune response and promote regeneration. They have great application potential in the treatment of rheumatoid arthritis and help improve the severity of rheumatoid arthritis.
Important research on stem cells in treating osteoarthritis and rheumatoid disease
Stem cells treat osteoarthritis, relieve pain and inflammation, and increase the thickness of articular cartilage
"Stem Cell Res Ther" reported a phase II clinical study "using allogeneic adipose mesenchymal stem cells to treat knee osteoarthritis." A total of 40 patients with knee osteoarthritis (KOA) were enrolled in this study and divided into two groups: stem cell group [20 patients received allogeneic adipose mesenchymal stem cells (AD-MSC)] and placebo group (20 patients received physiological saline). After 1 year of follow-up after treatment, the results showed:
1 Relief of inflammation
In patients in the stem cell group (ie, receiving AD-MSCs treatment), the serum levels of hyaluronic acid and cartilage oligomeric matrix protein were significantly reduced (P<0.05). Serum inflammatory marker levels dropped sharply after 3 months (P<0.001). During the 6-month follow-up, the expression of CD3, CD4, and CD8 showed a downward trend (P<0.05),(P<0.001), and (P<0.001) respectively.
2 Symptoms are relieved
① WOMAC Knee Function Score Scale: Compared with the placebo group, the total WOMAC score of patients in the stem cell group decreased significantly. After 6 months of stem cell treatment, the average score decreased by more than 70%(see the figure below for details).
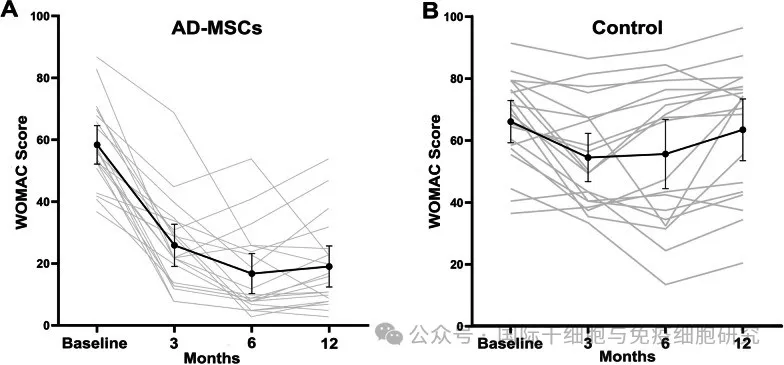
▲ Photo source "Stem Cell Res Ther"
② VAS score of knee pain: Compared with the placebo group, the VAS score of patients in the stem cell group showed a significant downward trend (see the figure below for details), indicating that the patient's pain symptoms were significantly reduced.
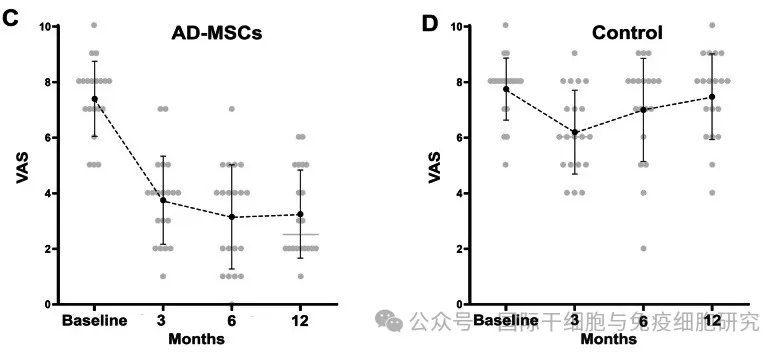
▲ Photo source "Stem Cell Res Ther"
③ SF-36 Quality of Life Scale: By comparing the scores of SF-36 scale, the health status of patients in the AD-MSCs group improved significantly (see the figure below for details).
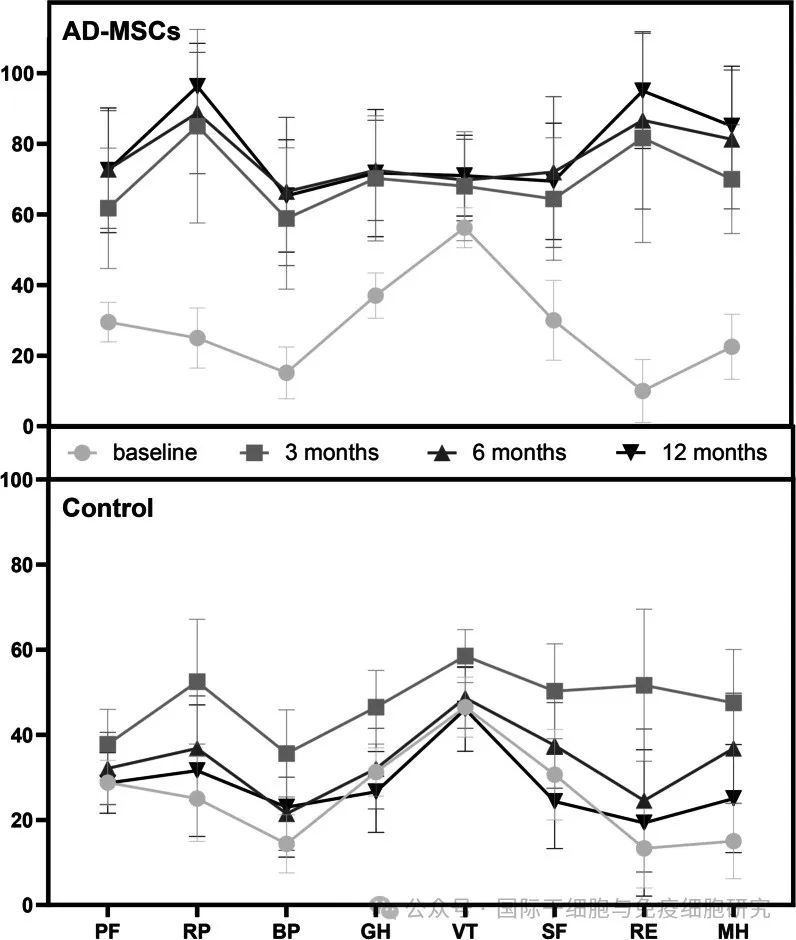
▲ Photo source "Stem Cell Res Ther"
Notes: PF-physical function;RP-physical role;BP-physical pain;GH-overall health;VT-vitality;SF-social function;RE-emotional role;MH-mental health.
3 Articular cartilage thickness
MRI showed that the thickness of tibial and femoral articular cartilage in patients in the AD-MSCs group increased slightly, especially in the medial posterior and medial anterior regions of the tibia (P<0.01 and P<0.05). Among them, the changes in one patient before and after AD-MSCs injection were as follows:
① Lateral anterior tibia (TLA) thickness: 2mm (before stem cell injection) vs 2.08mm (1 year after injection);
② Lateral central tibia (TLC) thickness: 1.76 mm (before stem cell injection) vs 1.79 mm (1 year after injection);
③ Lateral posterior tibial (TLP) thickness: 1.64 mm (before stem cell injection) vs 1.72 mm (1 year after injection);
④ The thickness of medial anterior tibia (TMA): 2.24 mm (before stem cell injection) vs 2.26 mm (1 year after injection);
③ The thickness of the medial center of the tibia (TMC): 2.51 mm (before stem cell injection) vs 2.65 mm (1 year after injection);
④ The thickness of the medial posterior tibia (TMP): 1.85 mm (before stem cell injection) vs 1.84 mm (1 year after injection).
▼ Comparison of MRI images of the tibial condylar cartilage in this patient before and 1 year after AD-MSCs injection
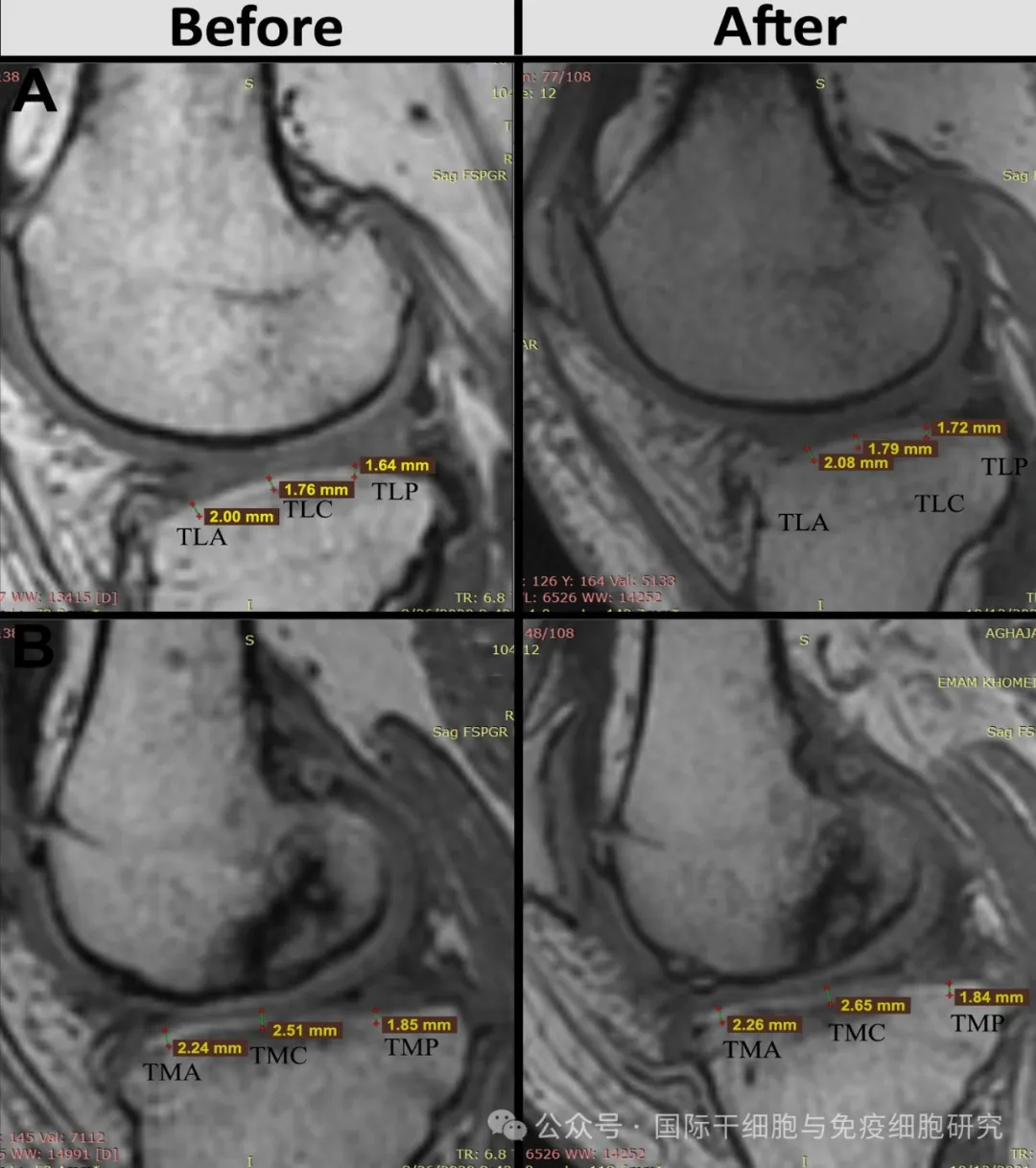
▲ Photo source "Stem Cell Res Ther"
The above results show that intra-articular injection of AD-MSCs is safe and feasible for the treatment of osteoarthritis. MRI results and clinical examinations show that articular cartilage regeneration and improvement in the treatment group are significant.
Joint swelling and tenderness improved after stem cell treatment for rheumatoid arthritis

▲ The screenshot comes from "BMC"
The journal Stem Cell Research and Therapy recently reported on a "I/IIa Clinical Study of the Use of Autologous Adipose Mesenchymal Stem Cells (AD MSCs) in the Treatment of Rheumatoid Arthritis (RA)(NCT03691909)". The study enrolled a total of 15 patients with rheumatoid arthritis aged between 18 and 65. After receiving autologous Adipose Mesenchymal Stem Cells treatment, the results showed:
1 Swelling joint count
Compared with pre-treatment baseline, swollen joint counts (as measured by the ACR 66/68 joint assessment) decreased significantly at each follow-up visit. At the end of follow-up at week 52, the swollen joint score improved significantly, with a median drop from 12.0 (IQR 8.0 - 19.0 before stem cell treatment) to 1 (IQR 0.0 - 3.0 at week 52), as detailed in the figure below.
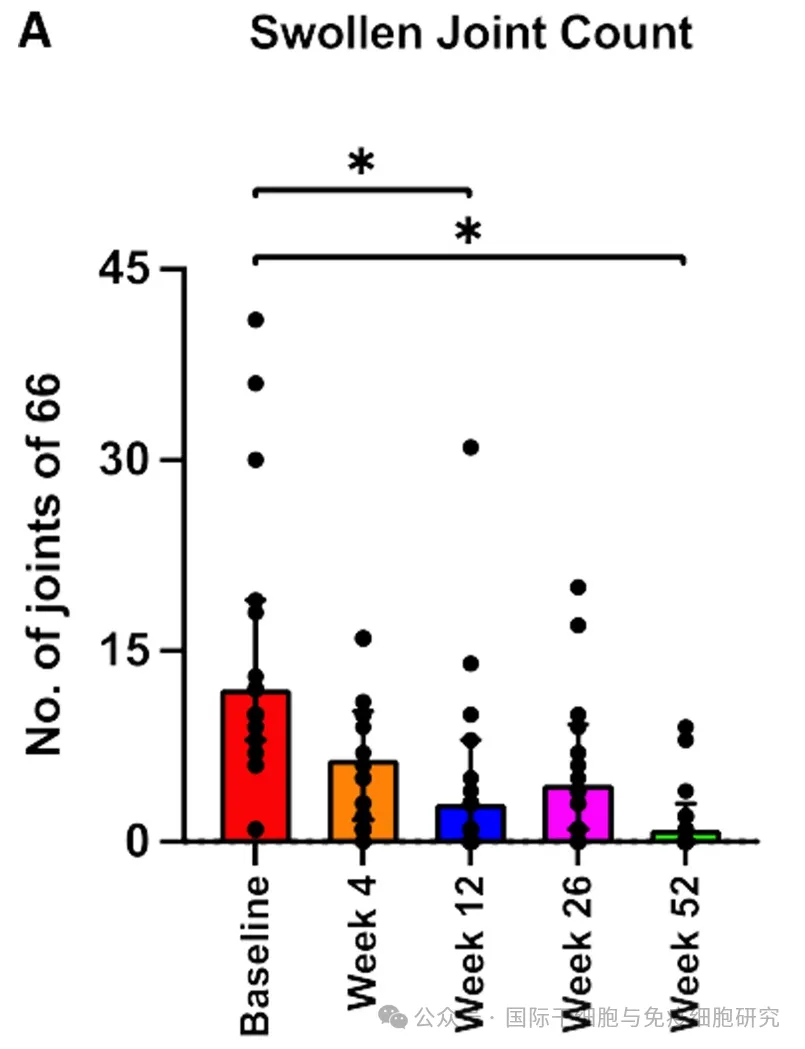
▲ Photo source "Stem Cell Research & Therapy"
2 Tender joint score
Compared with pre-treatment baseline, tenderness joint scores decreased significantly at each follow-up visit. At the end of follow-up at week 52, tenderness joint scores (as measured by the ACR 66/68 joint assessment) improved significantly, with a median drop from 20.0 (before stem cell treatment, IQR 11.0 - 36.0) to 1.0 (at 52 weeks of stem cell treatment, IQR 0.0 - 4.0), as detailed in the figure below.
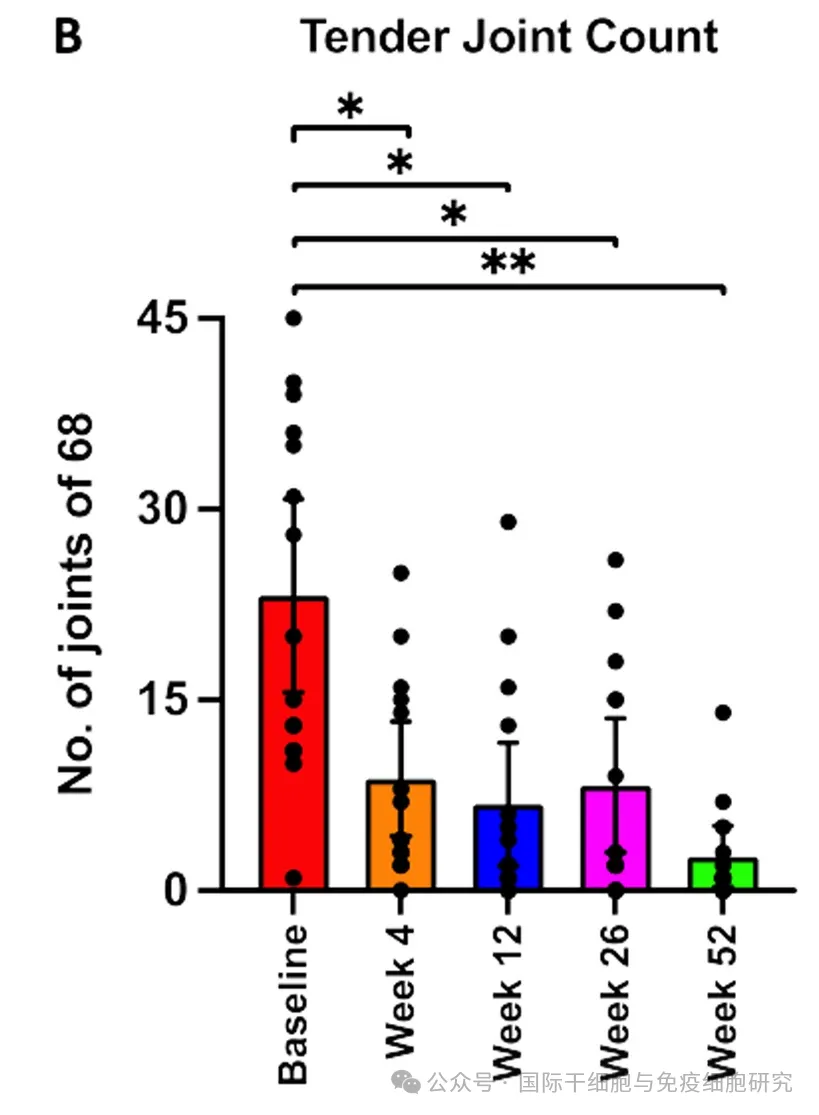
▲ Photo source "Stem Cell Research & Therapy"
The above results show that a single intravenous injection of autologous adipose mesenchymal stem cells can safely and effectively improve joint function in patients with active rheumatoid arthritis.
Summary
Osteoarthritis and rheumatoid arthritis have always been a long-standing problem in the field of bone and joint diseases. Currently, clinical treatment methods are limited, mainly focusing on symptomatic treatment. This is also an important opportunity for Australia to spend a lot of money to develop new therapies.
In recent years, with the continuous development of regenerative medicine, stem cell therapies with anti-inflammation, immune regulation, self-repair and other functions have gradually shown great application potential in the treatment of osteoarthritis and rheumatoid arthritis, helping to improve clinical symptoms, delay or organize disease progression, and improve patients 'quality of life! Xiao Bian also hopes that with the continuous deepening of research and development in various countries, more new therapies will be available in the future, benefiting more patients with bone and joint diseases!