
Source: Biological World
Our eyes produce tears to protect themselves from injury and infection. The conjunctiva is a tissue on the inner surface of the eyelid that covers the sclera (white of the eye). It contains two main cell types: goblet cells, which secrete mucus, and keratinocytes, which secrete tears. This mucus allows tears to stick to the surface of the eye and protects it from pathogens.
A number of diseases and illnesses can affect the conjunctiva, such as dry eyes, cancer, allergies and infections. In severe cases, dysfunction of the conjunctiva tissue can lead to blindness. Until now, there has not been a good model of the human conjunctiva, which has limited research into its function in disease and health. As a result, treatment options for diseases affecting the conjunctiva are also limited.
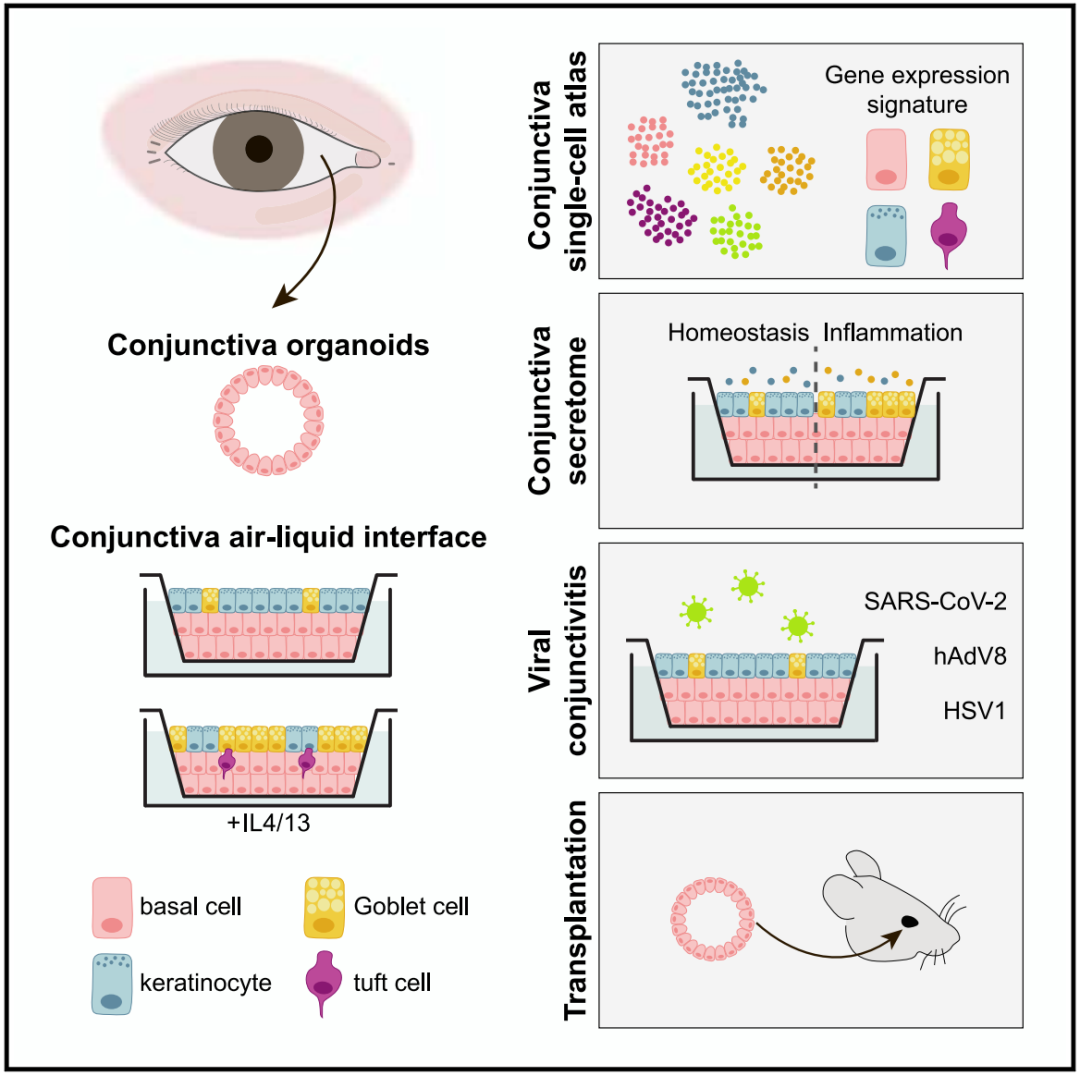
On January 11, 2024, Professor Hans Clevers' team published a paper in the journal Cell Stem Cell entitled: Human conjunctiva organoids to study ocular surface homeostasis and disease. The study developed the first human conjunctiva organoid model that mimics the function of an actual human conjunctiva, and using this organ model, the team identified a new cell type in the conjunctiva called tuft cells. Cluster cells are more enriched in allergy-like conditions and may therefore play a role in allergies. This conjunctival organoid model can also be used for drug testing for a variety of diseases affecting the conjunctiva.
In 2009, Hans Clevers et al. created the first intestinal organoids using adult stem cells from the mouse gut, ushering in an era of organoid research. Since 2009, research achievements in the field of organoids have continued, and many new and more complex organoids have emerged, enabling us to simulate the functions of various organs in the laboratory, which has brought more powerful tools for new drug research and development, precision therapy, regenerative medicine and other fields.
To gain insight into the composition and function of the human conjunctiva, the research team set out to develop the first human conjunctiva organoid model. They used cells from the human conjunctiva and grew them into 3D structures in petri dishes. These tiny structures are called organs and have the function of a real human conjunctiva.
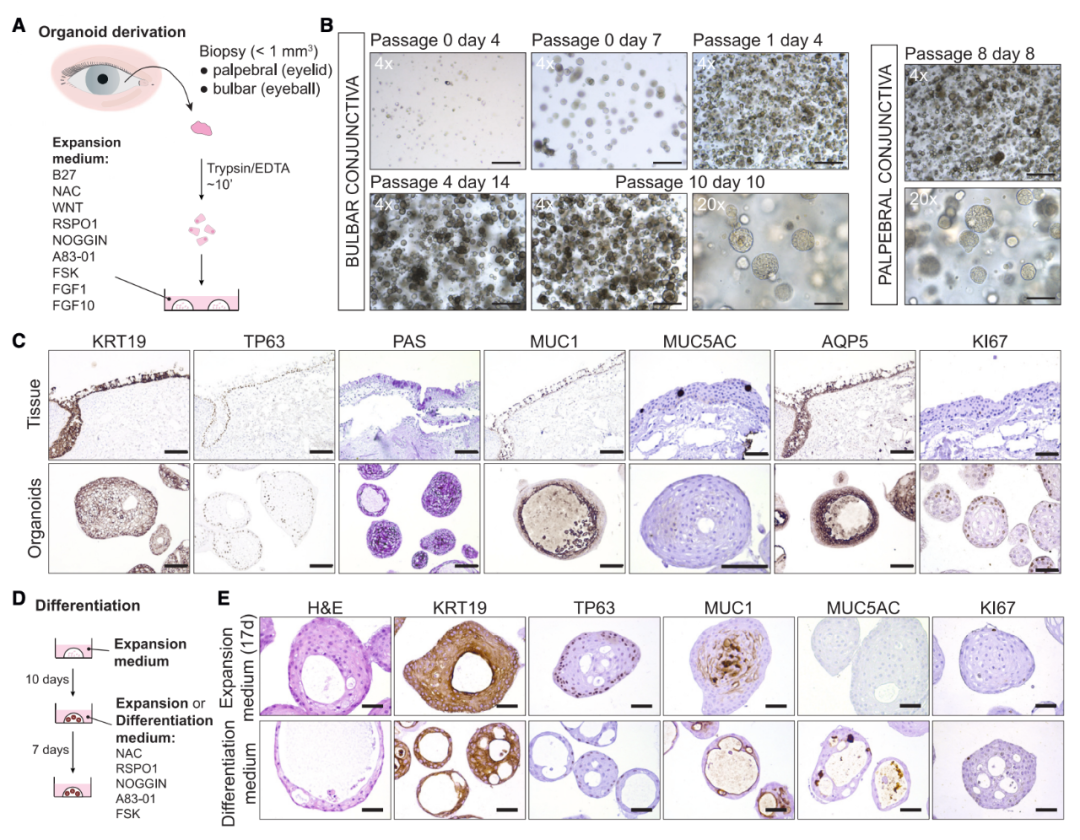 Establishment, characterization and differentiation of human conjunctival organoids
Establishment, characterization and differentiation of human conjunctival organoids
Having built a functional human conjunctiva organoid, the team wanted to shed more light on how the conjunctiva is involved in the production of tears. They found that the conjunctiva produces antimicrobial peptides and therefore promotes tear production in a number of ways, not just by making mucus.
Next, the research team changed the culture conditions of human conjunctival organoids to simulate an allergic reaction. The results showed that these organoids began to produce completely different tears: they produced more mucus, and they also produced more antimicrobial peptides. Under these conditions, they identified a new cell type called tuft cells in human conjunctival organoids. tuft cells Tuft cells have been found in a variety of tissues, but had not previously been found in human conjunctiva. The study found that clusters of cells become more abundant under allergy-like conditions, suggesting they play a role in the eye's response to allergies.
The study also found that human conjunctival organoids can be infected by herpes simplex virus type 1 (HSV1), human adenovirus type 8 (hAdV8) and novel coronavirus (SARS-CoV-2). Infection with HSV1 can be reversed by acyclovir, an anti-HSV drug, while infection with hAdV8, which lacks approved drug treatment, can be suppressed by cidofovir, an anti-cytomegalovirus drug. This suggests that human conjunctiva organoids can be used for drug research and screening for diseases affecting the conjunctiva.
Finally, the study showed that human conjunctival organoids can be transplanted into the conjunctival of mechanically damaged immunodeficient mice, and the research team is now conducting further preclinical validation on rabbits. According to the research team, this newly developed organoid model opens the door to the study of diseases affecting the conjunctiva, for example, we can use this model to test drugs for allergies or dry eyes, and in the long term, it may even be possible to create replacement conjunctiva for patients with eye burns, eye cancer or even hereditary blindness.
Paper link:https://www.cell.com/cell-stem-cell/fulltext/S1934-5909(23)00438-1