
A recent Japanese study has shown that heart spheres derived from human induced pluripotent stem cells can be easily transported and injected into damaged areas of the heart to promote its regeneration and functional recovery.
Regenerative heart therapy involves transplanting cardiomyocytes into damaged areas of the heart to restore lost function. However, it has been reported that there is a high risk of arrhythmia after this procedure.
The new study involved injecting "heart spheres" grown from human stem cells directly into damaged ventricles. The very positive results observed in primate models highlight the potential of this strategy.
Cardiovascular disease remains one of the leading causes of death worldwide and is particularly prevalent in developed countries. Myocardial infarction, commonly known as "heart attack," is on the rise, causing a large number of deaths each year.
A heart attack typically kills millions of heart muscle cells, leaving the heart in a weakened state. Because mammals cannot regenerate heart muscle cells on their own, heart transplantation is currently the only clinically viable option for patients with heart failure. Given that whole heart transplants are expensive and difficult to obtain donors, it is not surprising that alternative therapies have received high attention from the medical community.
One promising strategy that has been steadily gaining traction is the use of human-induced pluripotent stem cells (HiPSC) for regenerative heart therapy.
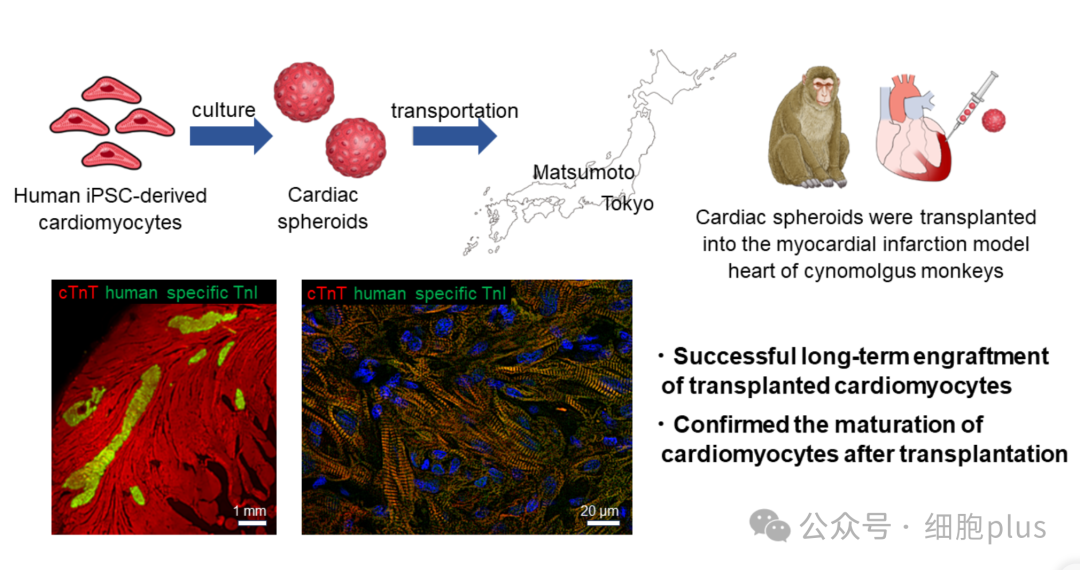
A Japanese research team from Shinshu University and Keio University School of Medicine has developed a new strategy for regenerative heart treatment that involves injecting "heart spheres" derived from HiPSC into monkeys suffering from myocardial infarction.
The study, published in the journal Circulation on April 26, 2024, was led by Professor Yuji Shiba of Shinshu University's Department of Regenerative Science and Medicine.

In their new method, the researchers grew HiPSC in a culture medium, causing them to differentiate into heart muscle cells. After carefully extracting and purifying cardiac spheroids (three-dimensional clusters of heart cells) from cultures, they injected about 6×10^7 cells into the damaged heart of a crab eating macaque (Macaca fascicularis).
They monitored the animals for 12 weeks, periodically measuring heart function. After that, they analyzed the monkeys' hearts at the tissue level to assess whether the cardiac spheres could regenerate damaged heart muscle.
First, the team verified the correct reprogramming of HiPSCs in heart muscle cells. Using electrical measurements at the cell level, they observed that the cultured cells exhibited the electrical potential pattern typical of ventricular cells. These cells also responded as expected to a variety of known drugs.
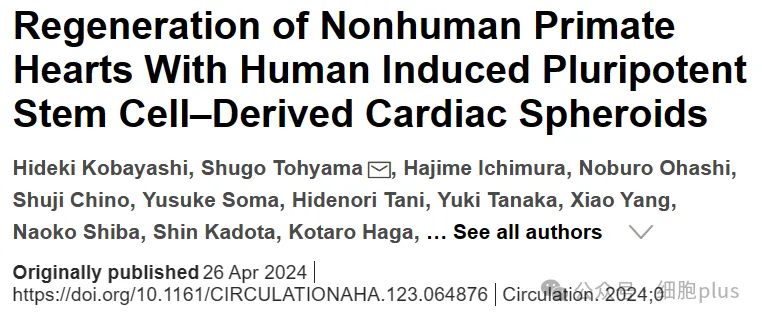
Most importantly, they found that these cells express adhesion proteins, such as connexin 43 and N-cadherin, in large quantities, which will facilitate the integration of their blood vessels into the existing heart.
The cells were then transported 230 kilometers from the Keio University lab to Shinshu University. The heart sphere is kept at 4°C for a four-hour journey. This means that extreme hypothermia measures are not required when transporting cells to the clinic, which will make future clinical procedures cheaper and easier to adopt.
Finally, the monkeys received either a cardiac sphere or a placebo injection directly into the damaged ventricles. During the observation period, the researchers noted that arrhythmias were very rare, with only two test subjects experiencing transient tachycardia (rapid pulse) within the first two weeks of the treatment group.
Using echocardiograms and computed tomography examinations, the team confirmed that the treated monkeys' hearts pumped their left ventricles better after four weeks compared to the control group, indicating a greater ability to pump blood.
Histological analysis eventually revealed that the heart graft had matured and was properly connected to pre-existing existing tissue, consolidating the results of previous observations.
According to the researchers, "HIPSC-derived cardiac spheroids are expected to be the best form of cardiac regenerative cardiomyocyte products due to their direct generation and effectiveness." We believe that the results of this study will help to solve the major problem of ventricular arrhythmia that occurs after cell transplantation, thus greatly accelerating the realization of cardiac regeneration therapy."
Although tested on monkeys, it is important to note that the cardiac globular production protocol used in this study was designed for clinical use in humans.
"The favorable results obtained to date are sufficient to give the green light for our clinical trial, known as the LAPiS trial." We have used the same cardiac sphere in patients with ischemic cardiomyopathy. "Professor Yuji Shiba said.
Reference:Regeneration of non-human primate hearts with human induced pluripotent stem cell-derived cardiac spheroids