
Multiple sclerosis (MS) is a chronic inflammatory and neurodegenerative disease that affects the central nervous system (CNS). Its pathogenesis is complex and involves the interaction of environmental factors (such as Epstein-Barr virus infection) and genetic factors. In the early stages of the disease, MS usually presents as local neurological symptoms caused by acute demyelinating lesions with some degree of endogenous repair (relapsing and remitting MS [RRMS]). Fewer patients (<15%) experience a continuously progressive course of disease (primary progressive MS [PPMS]) from the beginning of the disease, which is associated with a poor prognosis. Over time, most patients with RRMS develop secondary progressive MS (SPMS), which is characterized by a steady accumulation of neurological dysfunction associated with failure of repair mechanisms and neurodegeneration.
In RRMS, peripheral immune cell infiltration and inflammation are very evident, and treatment targeting B or T cells significantly reduces new lesions and recurrences. Unfortunately, these treatments have limited effectiveness in preventing neurodegeneration that drives disease progression, suggesting the existence of disease mechanisms independent of peripheral immunity. The mechanisms behind the progression of chronic MS are only partially understood, highlighting an urgent unmet need.
Single cell sequencing news: On August 26, 2024, the team of Dr. Valentina Fossati, senior research investigator from the Stem Cell Foundation (NYSCF) Institute in New York, and Case Western Reserve University Dr. Paul J. Tesla, director of the Institute of Glial Science at Case Western Reserve University, published a paper online titled "Patient iPSC models reveal glia-intrinsic phenotypes in multiple sclerosis" on Cell Stem Cell. The largest collection of stem cell models of multiple sclerosis (MS) patients has been created to date, and using advanced technologies such as single cell genomics, it has been discovered for the first time that glial cells of multiple sclerosis patients have intrinsic characteristics of the disease and are not affected by the immune system. Dr. Benjamin Clayton, assistant professor at Case Western Reserve School of Medicine, and Lilianne Barbar, a doctoral student at Washington University in St. Louis, were co-lead authors of the study.
The research team used the powerful capabilities of the NYSCF automated platform to create induced pluripotent stem cells (iPSC) from skin biopsies of multiple sclerosis patients, forming the largest multiple sclerosis patient stem cell line to date, covering different clinical subtypes. They then transformed iPSC into glial cells, including oligodendrocytes and astrocytes, to study their role in disease.
"The internal environment is constantly changed by immune cells and inflammatory signals. By generating glial cell-rich cultures from stem cells, we can study their role in MS independently of the complex internal environment." Dr. Fossati said.
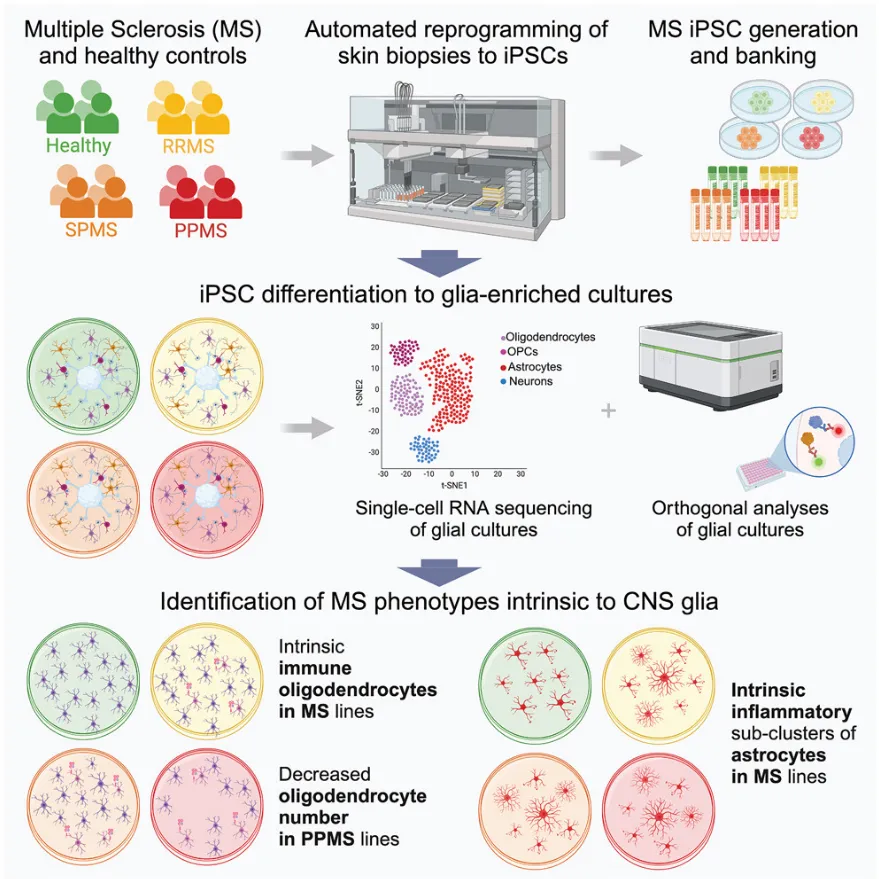
Through single-cell gene expression profiling, scientists found that stem cell-derived glial cell cultures from patients with primary progressive multiple sclerosis, a particularly serious disease, contained fewer oligodendrocytes. Oligodendrocytes are responsible for producing myelin sheath, the protective sheath around nerve fibers that is lost in multiple sclerosis.
Dr. Paul Tesla pointed out: "This observation challenges the traditional belief that multiple sclerosis is driven purely by immune system dysfunction, suggesting that the disease may also be triggered by biological processes in the brain itself."
The team also observed that a group of genes related to immune and inflammatory functions were particularly active in stem cell-derived glial cell cultures from multiple sclerosis patients, consistent with what they saw in brain samples from multiple sclerosis patients. In addition, NYSCF scientists used the latest technology of artificial intelligence to detect differences in astrocytes that are not easily perceptible to the human eye.
Due to the autoimmune activity of multiple sclerosis, many current therapies target the immune system. These drugs help reduce the frequency of immune attacks, but unfortunately they cannot stop the neurodegeneration that leads to disease progression.
The study's findings open up new possibilities for treating multiple sclerosis. By identifying the behavior of specific glial cells that cause disease, researchers can now explore potential therapies that target these cells directly, which may be more effective treatments than just suppressing the immune system.
The study's findings represent a major leap in understanding of multiple sclerosis and highlight the huge potential of glia as a target for therapeutic intervention, which may change the treatment prospects of many patients.
Original document: doi.org/10.1016/j.stem.2024.08.002