
Source: International Stem Cell Research
Although intracerebral hemorrhage accounts for only 10% to 20% of all strokes, it is a more dangerous type, and the American Heart Association and the American Stroke Association recommend supratentorial hematoma removal as a "life-saving" treatment for patients with severe intracerebral hemorrhage. However, many patients even after active treatment, smooth through the acute period, there may still be different degrees of sequelae, and there is no effective treatment, clinical rehabilitation treatment mainly, including rehabilitation function exercise, drug therapy (such as nutritional nerve drugs), physical therapy (such as transcranial magnetic stimulation) and other ways, but the effect is limited.
In recent years, with the continuous advancement of medical technology, stem cells have attracted considerable attention due to their potential nerve regeneration ability, and a number of preclinical and clinical studies have been conducted, providing a new therapeutic direction for functional recovery after cerebral hemorrhage!
What is cerebral hemorrhage and sequela of cerebral hemorrhage?
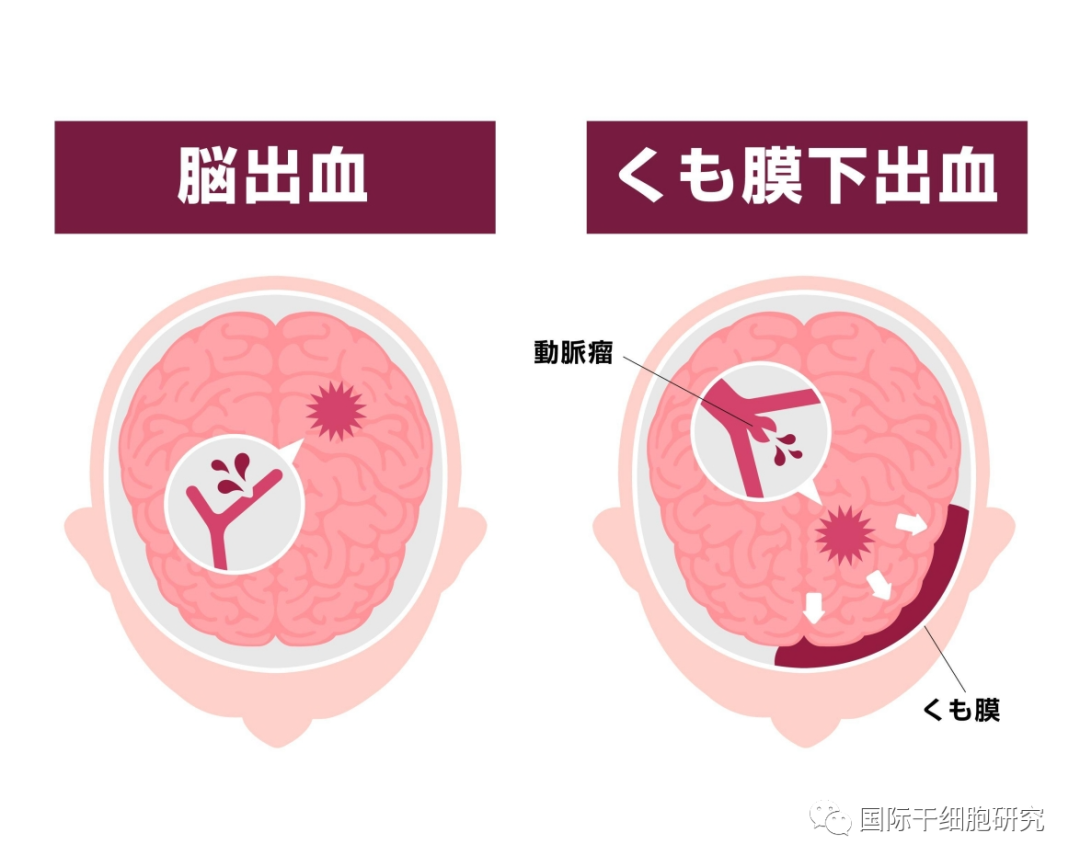
1、Cerebral hemorrhage
Cerebral hemorrhage (ICH), often referred to as "hemorrhagic stroke", refers to the spontaneous intracranial hemorrhage caused by the rupture of cerebral blood vessels due to a variety of reasons (such as hypertension, cerebral amyloid angiopathy, moyamoya disease, aneurysm, arteriovenous malformation, etc.), which can lead to brain tissue damage and neurological dysfunction, and its common symptoms include headache, nausea, vomiting, consciousness disorders, etc. According to the different anatomical location, cerebral hemorrhage can be divided into ventricular hemorrhage, cerebellar hemorrhage, brainstem hemorrhage (such as midcerebral ischemia, pontine hemorrhage, bulbar hemorrhage), basal ganglia hemorrhage (such as cerebral lobus hemorrhage, thalamic hemorrhage) and other common types.
2、Sequelae of cerebral hemorrhage
Sequelae of cerebral hemorrhage refer to the destruction of brain tissue and brain dysfunction caused by primary non-traumatic intracerebral parenchymal hemorrhage, mainly manifested as limb motor dysfunction (such as hemiplegia), speech disorder (such as aphasia), cognitive impairment, etc. The specific manifestations and severity of symptoms are related to the location and amount of cerebral hemorrhage, and the risk of disability in severe cases. Seriously affect the patient's health and quality of life.
The dysfunction after cerebral parenchymal hemorrhage arises not only from loss of neurons or synapses, but also from primary damage to white matter (WM) axons. Cerebral hemorrhage tends to occur in the basal ganglia and internal capsule (IC) region, which is rich in white matter (WM) fiber bundles that transmit sensory, motor, and visual information. Once bleeding occurs in this area, the physiological structure and function of WM will be interrupted to varying degrees, resulting in various functional disorders such as hemiplegia, hemianopia, and aphasia.
Clinical study of stem cell therapy for sequelae of cerebral hemorrhage
In recent years, stem cell therapy, represented by mesenchymal stem cells, has attracted much attention in the treatment of spinal cord injury, ischemic/hemorrhagic stroke and other neurological diseases, and a number of clinical studies have shown the expected results.
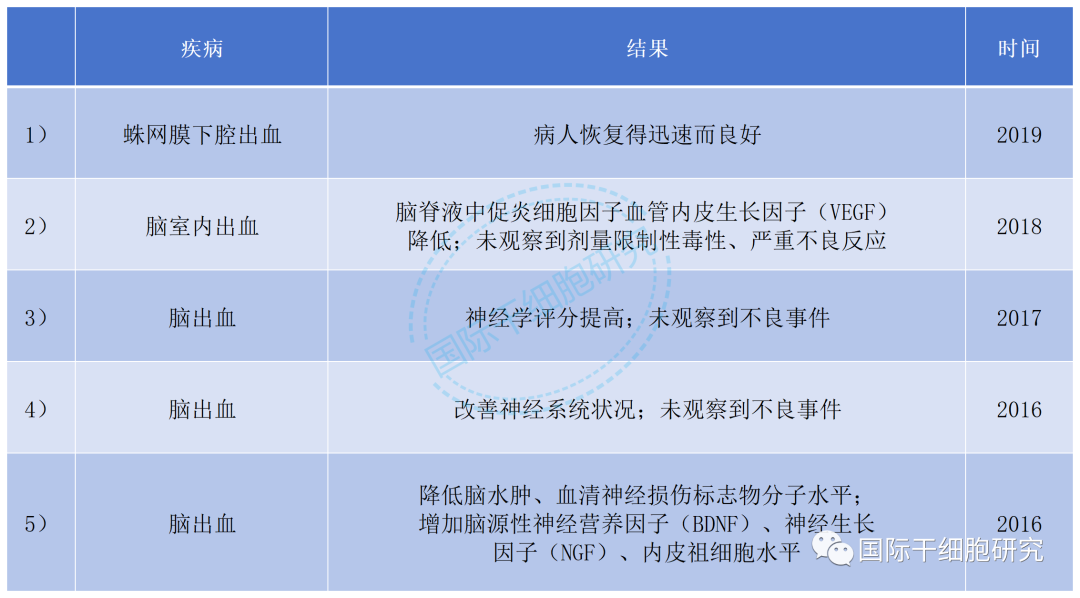
1、Clinical Study 1
According to Frontiers in Cellular Neuroscience, the first use of mesenchymal stem cells to treat the sequelae of cerebral hemorrhage was a case report of two patients with hemorrhagic strokes in persistent vegetative states (2016). Both patients received intraventricular injections of mesenchymal stem cells three times, each one month apart. After 1 year of follow-up, the results showed that the functional status of the two patients was significantly improved by the National Institutes of Health Stroke Scale (NIHSS) score.
2、Clinical Study 2
According to a clinical study reported in Cell Transplant, 206 patients with sequelae of cerebral hemorrhage were selected and divided into two groups. The patients in the transplant group were given mesenchymal stem cell (MSC) treatment through intrathecal transplantation; The other 96 cases were the control group. After one year of follow-up, patients in the transplant group showed significant improvements in their NIHSS (National Institutes of Health Stroke Scale) scores, Barthel index (a measure of functional status of the patient's activities of daily living), and mRS (Modified Rankin Scale) scores.
3、Clinical Study 3
A study reported the 5-year long-term follow-up results of stem cell transplantation for intracerebral hemorrhage. In this study, intracerebral hemorrhage patients with moderate to severe neurological impairment were selected and divided into three groups: BM-MNCs group (given autologous bone marrow mesenchymal stem cells), UC-MSC group (given umbilical cord mesenchymal stem cells) and control group. The results showed that both transplant groups had lower NIHSS (National Institutes of Health Stroke Scale) scores than the control group during a follow-up period of up to 5 years after transplantation.
However, at present, the treatment of cerebral hemorrhage sequelae by stem cells is still in the clinical research stage.
Table 1 Clinical study of stem cell transplantation in patients with cerebral hemorrhage
Why can stem cells treat sequela of cerebral hemorrhage?
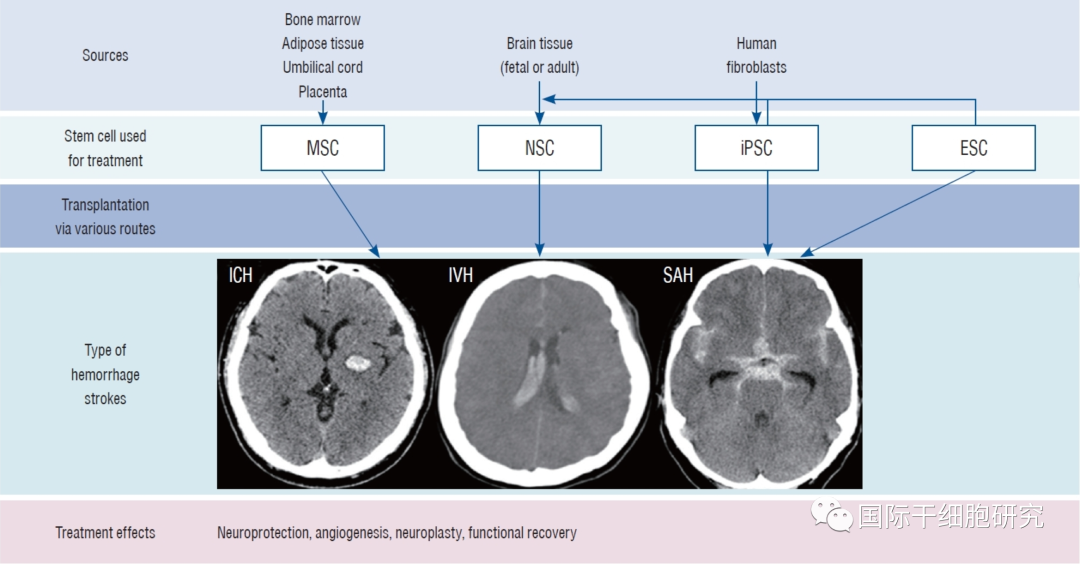
Mesenchymal stem cells (MSCS) are a class of self-renewing pluripotent stem cells that have the potential to differentiate into virtually any end-stage lineage and are essential for tissue homeostasis, repair, and regeneration. These cells can be obtained and expanded from a variety of adult and perinatal tissues, including bone marrow, adipose tissue, umbilical cord tissue, and peripheral blood. Bone marrow mesenchymal stem cells (BMSC), Japanese autologous fat MSC, and umbilical cord MSC are commonly used in clinical studies. According to previous studies, the influence mechanisms of stem cell therapy in the treatment of cerebral hemorrhage mainly include promoting the recombination of neural circuits, angiogenesis, improving the blood-brain barrier, anti-brain edema, anti-inflammation and neuroprotection.
1、Promotes the reorganization of neural circuits
Neurogenesis can be subdivided into exogenous and endogenous neurogenesis, where exogenous neurogenesis is the direct differentiation of implanted stem cells, while endogenous neurogenesis, mainly through stimulation of implanted stem cells, produces its own neuronal cells.
Studies have shown that after implantation of mesenchymal stem cells, patients improved in the ipsilateral coracofrontal region (auxiliary motor region) and the contralateral tail forelimb region (CFAA, primary motor region), which may be related to the reorganization of neural circuits.
2、Improve angiogenesis after cerebral hemorrhage
Angiogenesis is an important mechanism for the effectiveness of stem cell therapy because the brain tissue surrounding the hematoma is usually prone to ischemia. Studies have shown that angiogenesis is promoted by certain nutritional factors, such as vascular endothelial growth factor (VEGF), and implantation of mesenchymal stem cells can increase VEGF levels in the area around hematoma. It can also increase the level of CD31 (endothelial marker), regulate the response of endothelial cells to VEGF, and ultimately promote the recovery of nerve function by improving angiogenesis after cerebral hemorrhage.
3、Improve blood-brain barrier permeability
Secondary injury may occur after intracerebral hemorrhage, which is due to the further aggravation of neurological symptoms caused by peripheral edema. Therefore, reducing cerebral edema is an important strategy to prevent further progression of the disease. Studies have shown that the anti-brain edema mechanism of mesenchymal stem cells mainly includes two points, namely preventing the destruction of the blood-brain barrier and regulating the expression of AQP-4.
①Stop blood-brain barrier breakdown: Mesenchymal stem cells can help improve blood-brain barrier permeability by reducing levels of inducible nitric oxide synthase, 3-nitrotyrosine, matrix metalloproteinase-9 (which may disrupt the blood-brain barrier) and increasing levels of tight junction markers such as claudin-5.
②Regulate the expression of AQP-4: AQP-4 is the main water channel of the central nervous system, which is related to the pathogenesis of brain edema, and mesenchymal stem cells can down-regulate the expression of aquaporin-4 (AQP-4), thereby improving brain edema and ultimately preventing and improving secondary injury after cerebral hemorrhage.
3、Exert neuroprotective effects related to anti-apoptotic pathways
MSCs have certain neuroprotective effects, including anti-apoptotic or anti-degenerative functions, and thus help to improve the related manifestations of nerve damage in the sequelae of cerebral hemorrhage.
4、Reduce neutrophil infiltration and inflammatory macrophages
Inflammation can lead to secondary damage to intracerebral hemorrhage, so controlling inflammation is essential to prevent neurological deterioration of intracerebral hemorrhage.
Studies have shown that mesenchymal stem cells reduce the infiltration of neutrophils and the production of inflammatory macrophages by decreasing the levels of pro-inflammatory cytokines (such as interferon gamma, TNF-α (tumor necrosis factor α, IL-1 (interleukin-1), IL-2, IL-6) and increasing the levels of anti-inflammatory cytokines (such as IL-10). Finally, it can prevent and cure the sequelae related to cerebral hemorrhage caused by inflammation.
Peroration
Stem cell therapy is an emerging field developed in recent years, which can be differentiated into a variety of brain tissue cells, which helps to promote the recovery of neurological function, improve the quality of life of patients, and bring new hope for patients with sequelae of cerebral hemorrhage! However, the International stem cell Editor reminds us that in the acute phase of cerebral hemorrhage, timely medical treatment is needed to stabilize vital signs through traditional treatment methods such as surgery or drugs. After the condition is stable, other treatment methods can be considered to improve the sequelae.