
Source: BiG BioInnovation
When it comes to Parkinson's disease, many people's first reaction is: shake! Shake your hands!
But is Parkinson's just a shaking hand?
How is this common age-related disease diagnosed? What are the treatment options?
01 An introduction to Parkinson's disease
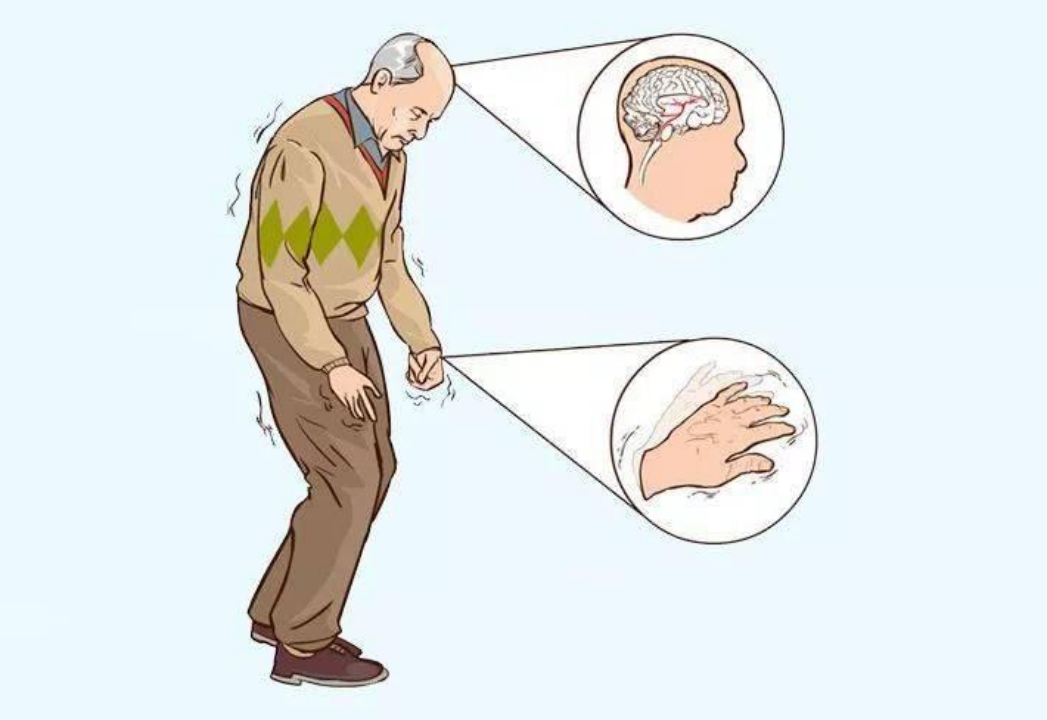
Parkinson's disease (Figure 1) is a chronic neurological disorder defined by the International Parkinson's and Movement Disorders Society (IPMDS) as: "a core clinical movement syndrome with dense neurodegeneration of the substantia nigra and synuclein deposition." Movement disorders caused by Parkinson's disease include: slow movement, paralysis tremor, involuntary movement, stiffness, difficulty walking, and imbalance; Non-motor symptoms include: impaired cognitive function, dementia, sleep disturbances, pain and sensory disturbances.
02 A diagnosis of Parkinson's disease
The original diagnosis of Parkinson's disease was based on the movement disorder of Parkinson's disease, and there are no physiological and biochemical tests to replace the diagnosis. Recent studies have shown that α-synuclein seed amplification assay can accurately distinguish Parkinson's patients from healthy controls, or can determine the stage of the disease. Alpha-synuclein seed amplification assays can identify people with Parkinson's disease early in the disease and even before symptoms appear, and a spinal tap can detect the presence of clumps of alpha-synuclein in the spinal fluid, a protein found in lewy bodies that is a microscopic marker of Parkinson's disease. At present, this Parkinson's disease test is only in the preclinical trial stage, patients have poor compliance phenomenon, the future also hopes to develop new biomarkers to define Parkinson's disease, or use blood samples instead of spinal fluid detection, in order to provide diagnostic basis for the diagnosis of Parkinson's disease on a biological basis.
03 Genetics and pathogenesis of Parkinson's disease
IPMDS, in its research on the genetics of Parkinson's disease, proposes that individuals who carry partial genetic mutations are more likely to develop Parkinson's disease. There are currently seven genes designated as single-gene triggers, four of which cause late-onset autosomal dominant disorders (LRRK2, CHCHD2, VPS35, and SNCA) and three cause early-onset autosomal recessive disorders (PARKIN, DJ1, and PINK1). In addition, mutations in the gene GBA are defined as the most common genetic risk factor for Parkinson's disease, with penetrance of up to 30%. However, genetic testing cannot be used as a diagnostic criterion for Parkinson's disease, but it can help predict a family member's risk of developing the disease.
In recent years, the research on the pathogenesis of Parkinson's disease has gradually deepened, and the research shows that the mutation of NR4A2 gene is related to the onset of Parkinson's disease. NR4A2 gene is a transcription factor, and the mutation will lead to the dysfunction of dopaminergic neurons, and then trigger the symptoms of Parkinson's disease.
In addition, the loss of mitochondrial DNA and the mutation of the LRRK2 gene have also been implicated in the pathogenesis of Parkinson's disease, and the loss of mitochondria, which are the main sites of energy production within the cell, leads to insufficient energy supply, which in turn impaffects the function of dopaminergic neurons. Mutations in the LRRK2 gene lead to abnormal protein accumulation, which can trigger cytotoxic reactions. These findings provide important clues to the pathogenesis of Parkinson's disease.
Epidemiological studies of Parkinson's disease have shown that geographical and ethnic differences play a role in its incidence. The prevalence of Parkinson's disease is significantly higher in Caucasians than in other ethnic groups and is higher in the northeastern and Midwest regions of the United States. This phenomenon may be related to the interaction of genetic factors and environment. In addition, some studies have found that people who are chronically exposed to environmental pollutants such as pesticides and heavy metals have a higher risk of developing Parkinson's disease. These epidemiological data provide a reference for the prevention and control of Parkinson's disease.
04 Prospects for future treatment of Parkinson's disease
There is no cure for Parkinson's disease, but medication, surgery and rehabilitation can be used to reduce symptoms. China released the "Guidelines for the Treatment of Parkinson's Disease in China" in 2020 (Figure 2). The drugs for the treatment of Parkinson's disease include compound levodopa, dopamine receptor agonists, anticholinergics and amantadine. Although dopamine replacement therapy remains the gold standard of Parkinson's disease treatment, the impact of movement disorders on patients' lives bodes well for the need for new treatments in the future.
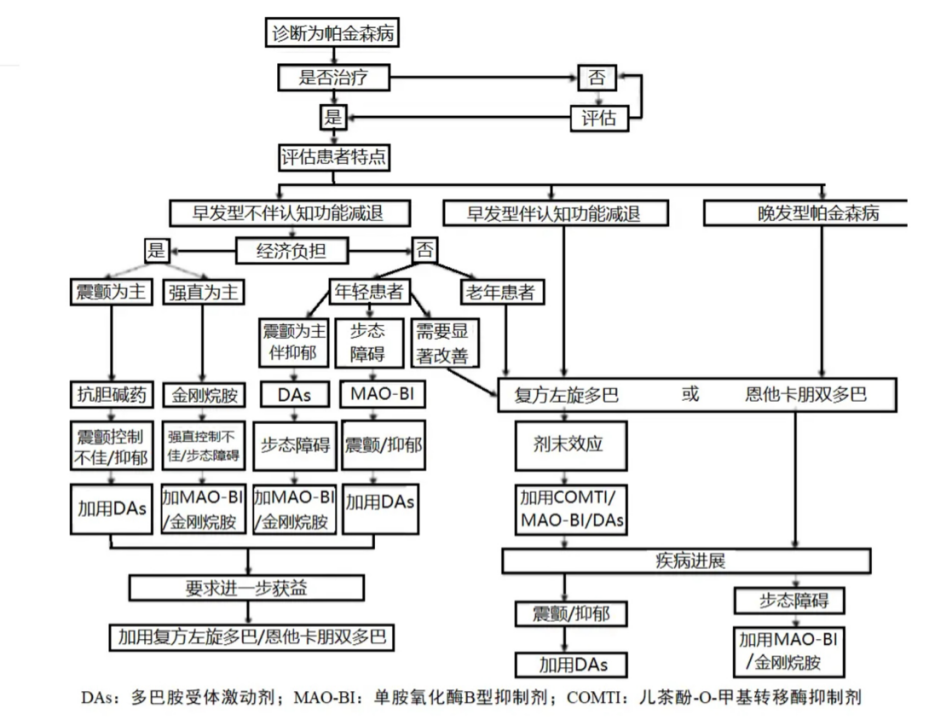 FIG. 2 The treatment process of Parkinson's disease The picture is from the Chinese Parkinson's Disease Treatment Guide.
FIG. 2 The treatment process of Parkinson's disease The picture is from the Chinese Parkinson's Disease Treatment Guide.
Neuroregulatory technology is widely used in the rehabilitation of Parkinson's disease, non-invasive neuroregulatory technology uses physical and chemical factors such as sound, light, electric current or magnetic field to stimulate the central nervous system and peripheral nervous system to improve the symptoms of the disease. Among them, repetitive transcranial magnetic stimulation (rTMS) and transcranial direct current stimulation (tDCS) are the most commonly used non-invasive neuroregulatory techniques. rTMS enhances the excitability of the cerebral cortex by stimulating neurons in the brain, or improves motor and non-motor symptoms such as cognitive impairment, sleep disorders, and depression by repairing abnormal neuroplasticity. Studies have shown that rTMS can increase the effectiveness of motor balance training and improve overall cognitive function in patients with Parkinson's disease. In addition, rTMS combined with medication can significantly improve clinical outcomes in patients with Parkinson's disease and can improve motor symptoms and cognitive dysfunction. tDCS regulates neuronal excitability by applying a weak current to specific brain regions. Studies have found that in people with Parkinson's disease, tDCS can assist movement, improve balance and walking ability, and regulate excitability in the prefrontal cortex, thereby improving cognitive function and gait disorders. In addition, tDCS can be combined with computer-assisted cognitive rehabilitation training to improve cognitive function in patients with Parkinson's disease.
In recent years, the application of robot science in the medical field has also achieved good results. In the field of rehabilitation medicine, robots can be divided into four categories: self-care support robots, nursing support robots, training support robots and employment robots. Among them, the training support robot is a kind of technology to carry out auxiliary or alternative training after wearing the robot, and the training support robot is the most widely used in the rehabilitation treatment of Parkinson's disease. For example, training of Gait Trainer GT1 training support robot for patients with HY Grade 3 Parkinson's disease showed that compared with conventional rehabilitation training methods, robot training can improve the walking speed and balance ability of patients with Parkinson's disease, but there is no significant difference in gait automaticity. A month of training supporting robotic training in Parkinson's patients with HY grade 2 and above found that robotic training had advantages over conventional rehabilitation methods for Parkinson's patients with frozen gait, similar to previous findings. In addition, studies have reported the use of robotic training in upper limb dysfunction in patients with Parkinson's disease. For example, using the Bi-Mnu-Track robot for upper limb training, it was found that the motor function and flexibility of the upper limb were improved. A randomized controlled trial of semi-autonomous exoskeleton training in hospitalized patients with Parkinson's disease found that robotic training significantly improved upper limb flexibility, executive function, and overall quality of life in patients with Parkinson's disease.
In general, as a new treatment technology, the robot training system can objectively and accurately control training and movement parameters, and can stably and safely perform repeated training and provide real-time feedback.
05 Sum up
Research institutions and medical experts are working on Parkinson's research and treatment, exploring new treatments, finding more effective drugs, developing innovative rehabilitation and support programs, and increasing public awareness and understanding of Parkinson's disease. The future treatment of Parkinson's disease will continue to explore the integrated application of multiple treatment modalities, and provide patients with more effective treatment and rehabilitation programs through continuous progress in science and technology and innovation in medical models, so as to better cope with the global challenges of Parkinson's disease.