
Data show that there are about 8.9 million patients with heart failure in China, and nearly half of them die within 5 years after the diagnosis of heart failure. Their 5-year survival rate is lower than that of most malignant tumors. In the past, heart failure could not be cured, and medical methods could only delay the progression of the disease. In recent years, with the advancement of science and technology, patients with heart failure have welcomed new treatment methods.
In May 2020, the journal Nature reported that two patients with end-stage heart failure received heart failure treatment based on reprogrammed stem cells in China and recovered and discharged one year later. It is reported that the patient was injected with cardiomyocytes differentiated from iPSC in May 2019, which is the world's first known clinical application of iPSC technology to treat damaged hearts.
iPSC (induced pluripotent stem cells), i.e. induced pluripotent stem cells, refer to a type of pluripotent stem cells that are artificially reprogrammed and cultured by reverse differentiation. iPSC has multi-directional differentiation and strong self-replication potential. Under certain conditions, it can differentiate into multiple functional cells, and millions or even billions of clinically relevant phenotypic cells can be cultured in vitro.
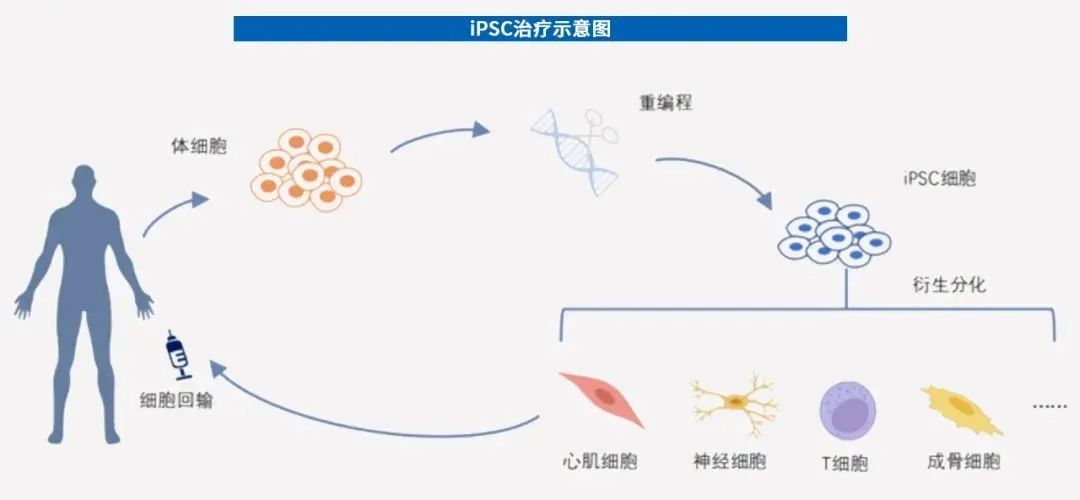
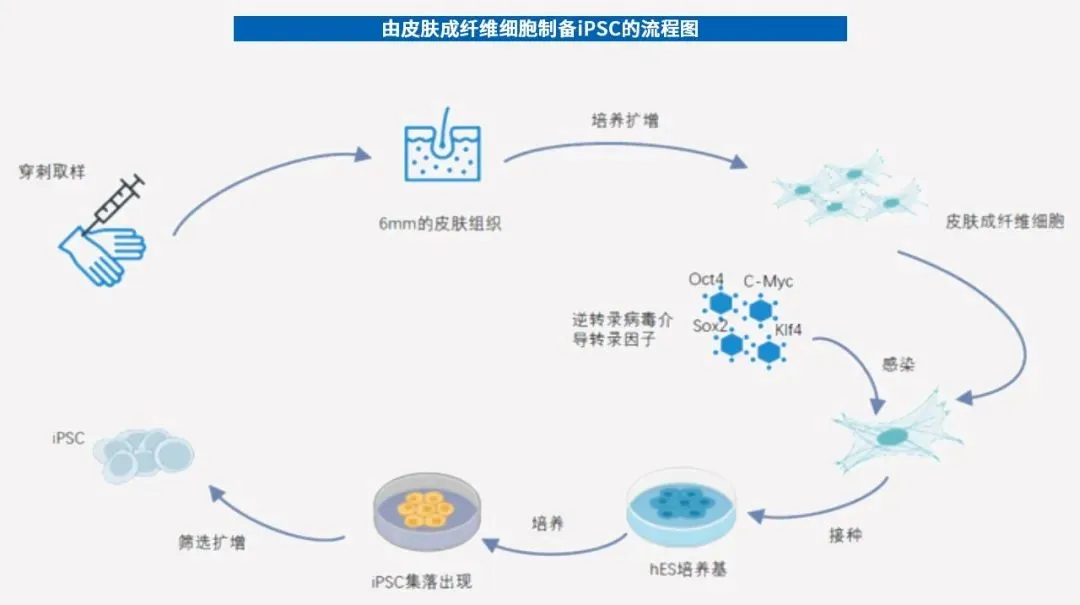
Researchers obtain somatic cells (such as fibroblasts) for in vitro reprogramming and inducing them into iPSC, which are then derived and differentiated into target cells (such as cardiomyocytes, etc.), and then transplanted into patients to achieve the effects of repairing tissue and enhancing immunity. In 2006, Professor Nobuya Yamanaka of Kyoto University in Japan used a viral vector to transfer a combination of four transcription factors (Oct4, Socx2, Klf4 and c-Myc) into mouse skin cells, successfully inducing iPSC. Therefore, Nobu Yamanaka won the 2012 Nobel Prize in Physiology or Medicine six years later. Later, large-scale research on iPSC was launched on a global scale.
At present, iPSC has been tried in the clinical treatment of diseases, with indications including heart failure, stroke, knee osteoarthritis, Parkinson's disease, leukemia, etc. In April 2022, China approved an iPSC-derived cell therapy product to enter clinical trials for the first time. In addition, iPSC can also be used for drug screening CRO (R & D outsourcing) services on the pharmaceutical side and disease models on the scientific research side.
In the era of cell therapy, iPSC may become the optimal solution
In 2015, the famous cancer doctor and writer Siddhartha Mukherjee mentioned in his speech "Forget the Pills, Cell Therapy is Coming" that drug treatment has brought about a huge change in human history, allowing pneumonia, syphilis, and tuberculosis. and other diseases can be cured. The model of drug treatment is-"disease, drug, target". For example, if you are infected with pneumonia, you can take penicillin to kill microorganisms. However, models of drug treatment for disease do not always work. Nature provides another perspective on disease: cells combine into organs, and organs aggregate into life, ultimately building rich ecosystems. Mukherjee believes that for a large number of diseases caused by non-infections, including chronic degenerative diseases such as diabetes, hypertension, and heart disease, what people may need to do is to "cultivate something", that is, cells.
The model of cell therapy is: "cell, tissue, environment." Cell therapy will become one of the important methods of disease treatment in the future. It has a unique mechanism of action. Its main advantages are: significant and lasting efficacy, personalized treatment, and treatment of diseases that are not treatable in traditional drug treatment methods. It is generally believed that cell therapy includes immune cell therapy, stem cell therapy, and other cell therapies.
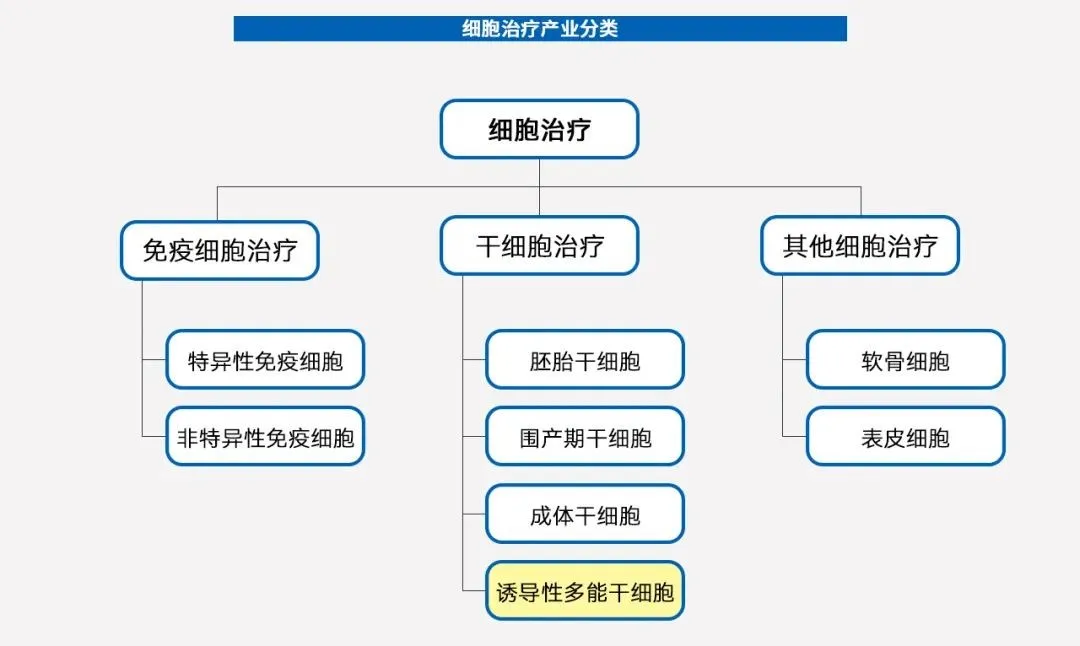
In the cell family, stem cells are builders and repairers, and immune cells are defense forces. They work together to create a healthy human body. When the human body is still growing, stem cells increase the type and number of cells by constantly dividing and differentiating new cells; when the body no longer grows after adulthood, stem cells can replace and replace aging or damaged cells in time; When foreign enemies (such as bacteria and viruses) invade, or traitors appear internally (such as normal cells mutate into cancer cells), immune cells will quickly recognize and eliminate them. As far as stem cells are concerned, they can be divided into embryonic stem cells, perinatal stem cells and adult stem cells according to their source.
l Embryonic stem cells are stem cells isolated from embryos;
l Perinatal stem cells are stem cells extracted from tissues such as cord blood, cord, and placenta attached to the fetus at birth;
l Adult stem cells are stem cells extracted from adult body tissues, such as bone marrow, fat, nerves, skin, etc.
In the words of a scientist,"Adult stem cells are like the trunk of a big tree, and embryonic stem cells are like the roots of a big tree. Embryonic stem cells not only maintain unlimited self-renewal characteristics, but also can differentiate into various tissue cell types in the body. They are considered to be the 'universal cells'with the most clinical application value." However, because embryonic stem cells need to be extracted from embryos, there are ethical risks when used in clinical applications. iPSC has the differentiation potential similar to embryonic stem cells and can be induced by adult human cells. It solves the long-standing ethical problems faced by regenerative medicine and the rejection reaction caused by allogeneic transplantation. It has convenient sources and has both universal and personalized treatment. Product capabilities have broader application prospects.
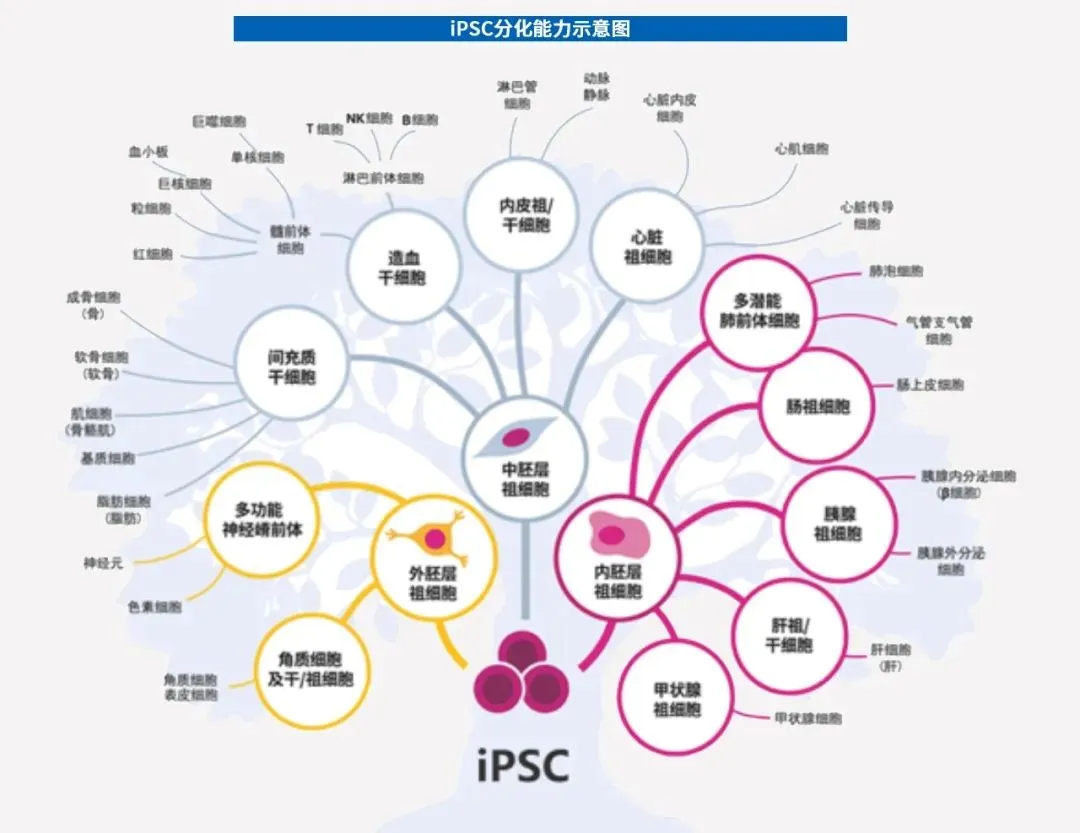
iPSC can also differentiate into immune cells. At present, cell therapies such as CAR (Chimeric Antigen Receptor)-T, CAR-NK, and CAR-M derived from human iPSC have been available and have begun to gradually transform into clinical practice. A milestone event was that in October 2020, the research team from the Institute of Physics and Chemistry of Chiba University in Japan announced that it had successfully completed the world's first transplant operation to transplant NKT cells based on iPSC differentiation into cancer patients. This is also Japan's first attempt to use iPSC to treat tumors. Currently, immune cell therapy products that have entered clinical application basically use patients 'autologous immune cells as raw materials. Autologous immune cell therapy products are highly personalized, have limited production scale, difficult quality control, long preparation cycles, and cannot benefit patients with rapid disease progression. Through iPSC technology,"off-the-shelf" immune cell therapy products from allogeneic origin can be prepared to reverse body damage or disease. iPSC can also be used to grow organoids.
iPSC can be combined with gene editing technologies such as CRISPR to accurately and directionally perform gene knockouts or knockins in many types of cells, including single base changes, correct genetic errors within the stem cell genome, and add new ways to personalized medicine. As an emerging technology, iPSC "strings" technologies such as immune cell therapy, stem cell therapy, and even organoid culture and gene editing, showing huge application potential. For now, iPSC may be the best cell therapy option.
In theory, any type of somatic cell can be easily reprogrammed, but iPSCs are basically prepared from easily accessible cells, such as cells from skin or blood. Taking the classic four-factor method as an example, the preparation of iPSC mainly involves four major steps: isolation and culture of somatic cells → construction of mediated vectors → introduction of inducing factors and cell culture → screening and identification of iPSC.
At present, many countries and regions have established iPSC super donor banks, and China also completed the preparation of the first pluripotent stem cell strain induced by a "super donor" in 2018. Similar to the United States, China's population has complex HLAs, and its super donors can only cover about 50% of the Chinese population. Therefore, it is necessary to establish a personal iPSC library as a future reserve.