
Source: Cell plus
Encouraging results from a trial of a new stem cell-based treatment, published in Nature Biotechnology at the end of November 2023, have led experts to believe that in the future, people with type 1 diabetes will no longer need to receive daily insulin injections, and stem cells are "a matter of time."
The trial involves a subcutaneous implant that encapsulates stem cells in place of an artificial insulin injection.
A Canadian clinical trial conducted by the University of British Columbia (UBC) and Vancouver Coast Health (VCH) found that the therapy can regulate blood sugar levels and reduce the need for daily insulin injections.
Dr David Thompson, principal investigator at the Vancouver Trial Centre, Professor of Endocrinology at UBC and director of the Diabetes Centre at Vancouver General Hospital, said: "This is an important step towards a functional cure for type 1 diabetes.
"For the first time, a stem cell-based device can reduce the amount of insulin used in some patients with type 1 diabetes. With further refinement of this approach, it is only a matter of time before we find a therapy that can completely eliminate the need for daily insulin injections."
The device, called VC-02 (from ViaCyte, a company we described earlier and now merged with Vertex), is designed to deliver a long-term steady stream of insulin carrying millions of beta cells cultured from pluripotent stem cells.
Co-author Dr. Timothy Keefer, a professor in UBC's Department of Surgery and Cellular and Physiological Sciences, said: "Each device is like a miniature insulin production factory, with islet cells grown from stem cells packed into the device to fundamentally re-establish the blood sugar regulation function of a healthy pancreas. Given that we can create an almost unlimited supply, this could have huge benefits over transplanting hard-to-obtain donor cells."
The trial included 10 participants who were unable to self-produce insulin at the start of the study.
After six months, significant markers of insulin production were found in three participants (Figure 1, 2, and 3 below), and the levels remained unchanged for the remainder of the 12-month study.
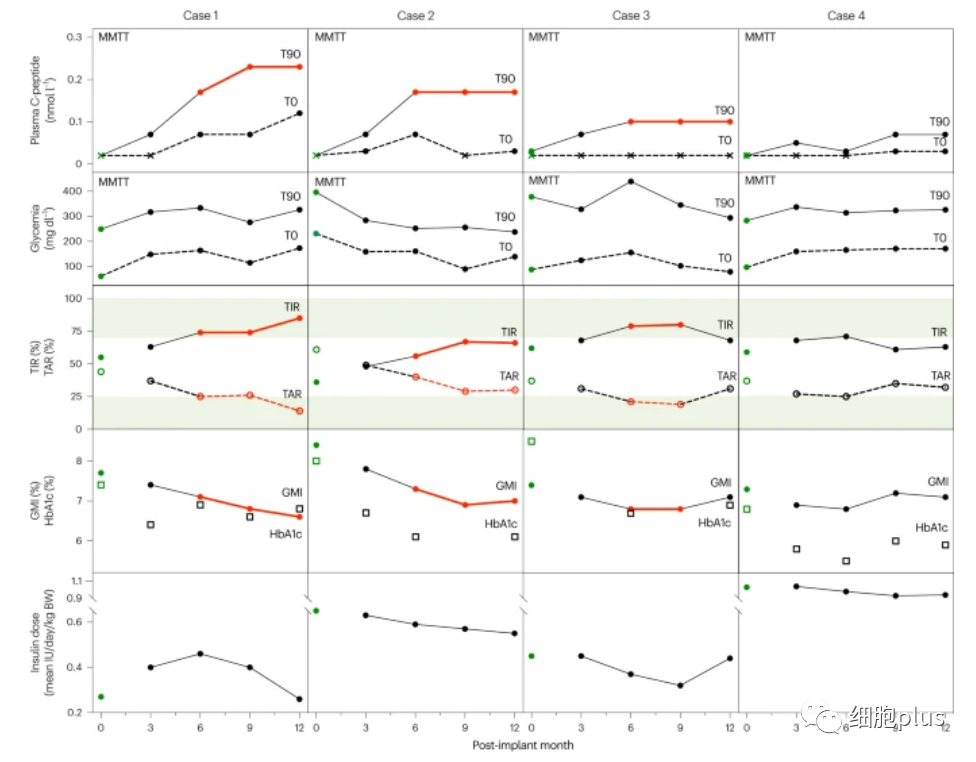
In the figure above, cases 1, 2, and 3 achieved the secondary efficacy endpoint for implant function (plasma C-peptide > 0.07 nmol l−1) and were maintained until month 12 (red line). Three recipients (cases 1, 2, and 3) who met the secondary endpoints of implant function had improved CGM measurements toward clinical goals at 6 and 9 months, and two of them also improved at 12 months (red line). Improvements in the glucose control endpoints in cases 1, 2, and 3(red line) were associated with lower insulin doses.
In addition, the three participants reduced the amount of insulin they needed to inject.
One participant increased his glucose target range time (TIR) from 55 percent to 85 percent and reduced his daily insulin dosage by 44 percent.
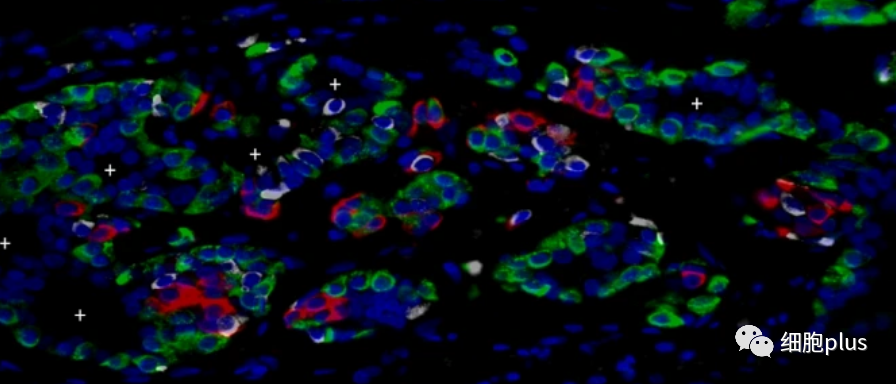
Immunohistochemical analysis of the implants at 6 months showed insulin (red), glucagon (green), CD34(white) and DAPI(blue).
The trial was funded by the Canadian Stem Cell Network and SCN is proud to play its part and looks forward to the next step in game-changing diabetes research.
The researchers are conducting another trial to test whether another version of the kit could eliminate the need for immunosuppressive drugs during treatment, using modified cells to evade the immunosuppressive immune system.
Dr. Thompson said, "We envision a future in which people with type 1 diabetes will be able to live without the need for daily insulin injections and immunosuppressive medications. That future is now within reach, and Canada is leading the effort to bring these new therapies to patients."