
Parkinson's Disease is a common degenerative disease of the central nervous system that mainly affects middle-aged and elderly people, with millions of patients worldwide. Typical symptoms include tremors, muscle rigidity, slow movements and unstable posture, which have a serious impact on the patient's quality of life. As the population ages, the number of Parkinson's disease patients in China is also increasing year by year, and more effective treatment methods are urgently needed.
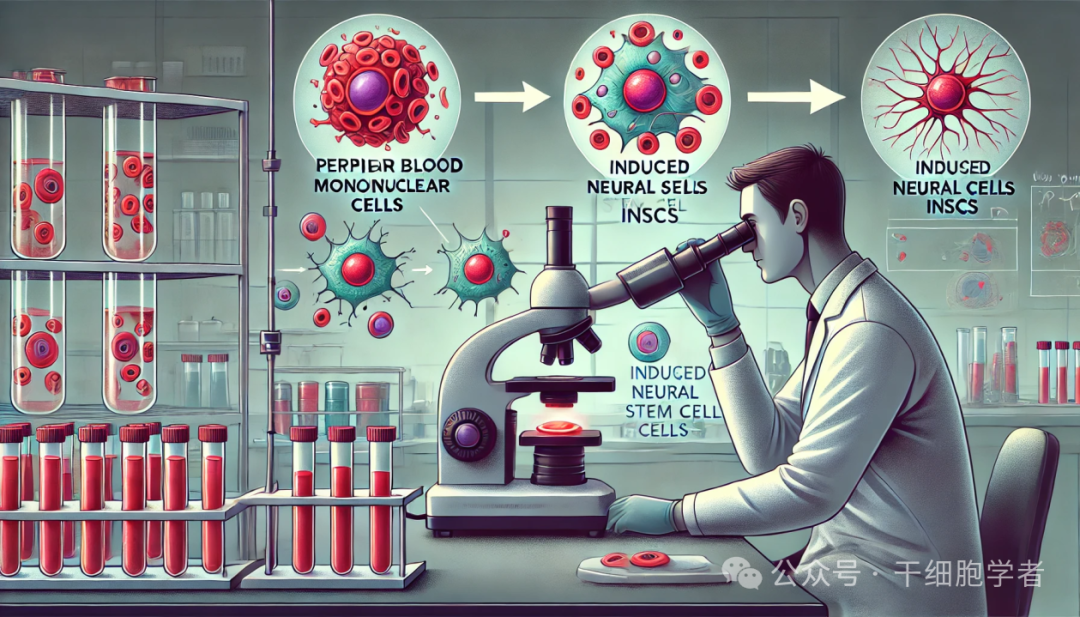
Faced with this medical challenge, Xuanwu Hospital took the lead in conducting an innovative study using autologous induced neural stem cell (iNSC) technology to treat Parkinson's disease, and showed significant efficacy in 12 months of clinical observation. This technology uses the patient's own peripheral blood mononuclear cells (PBMC) to directly transform them into neural stem cells, which then produce dopaminergic neural precursor cells through directed differentiation, thereby replacing damaged neurons in the brain.
Clinical status and challenges of Parkinson's disease
The pathogenesis of Parkinson's disease is closely related to the degeneration of dopaminergic neurons in the substantia nigra of the midbrain. This degeneration leads to insufficient dopamine secretion, which can cause motor control disorders. Although the medical community currently uses drugs, surgery and rehabilitation methods to alleviate symptoms, such as levodopa (LDOPA) therapy, patients still often experience "dose wear" effects and exercise complications after long-term use.

Most existing treatments focus on symptom control rather than fundamentally reversing the disease. Surgical therapies, such as deep brain stimulation (DBS), can provide relatively stable symptom relief in some patients, but their limitations are narrow indications and require complex postoperative management.
Autologous induced neural stem cell (iNSC) therapy has demonstrated revolutionary therapeutic prospects with its unique autologous origin and low immune rejection rate. This method effectively avoids immune rejection and ethical controversy by using the patient's own cells, providing possibilities for long-term and stable disease management.
Principle and process of autologous induced neural stem cells (iNSC) in the treatment of Parkinson's disease
The core of autologous induced neural stem cell (iNSC) therapy is to transform the patient's own peripheral blood mononuclear cells (PBMC) into neural stem cells, and then through targeted induction, these stem cells can be differentiated into dopaminergic neural precursor cells and implanted into the patient's brain. This process not only restores dopamine secretion, but also directly interferes with the disease process through cell replacement. Specifically, the technical process of this therapy includes the following steps:

Peripheral blood mononuclear cells (PBMC) collection and iNSC preparation
During the treatment process, peripheral blood is first extracted from the patient, and monocytes in the peripheral blood are obtained through isolation techniques. As an easy source of autologous cells to collect, PBMC avoids possible immune rejection problems caused by allotransplantation. Under in vitro culture conditions, these PBMC are transformed into iNSC, neural stem cells with multi-directional differentiation potential. Through this induction process, the research team successfully prepared iNSC with a controllable number and efficient differentiation ability.
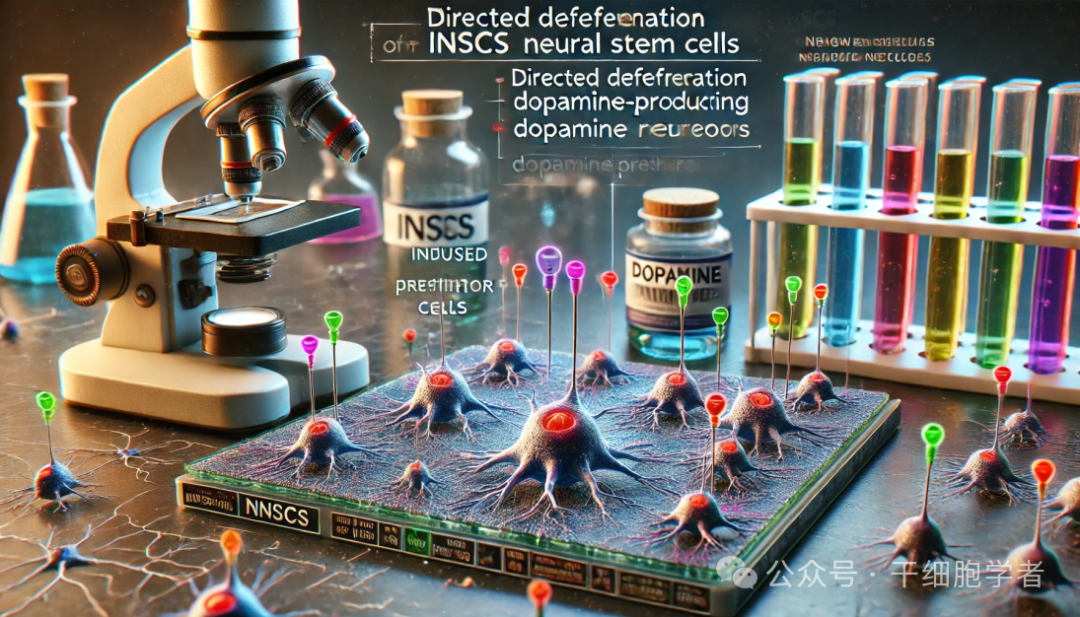
Directed differentiation of dopaminergic neural precursor cells
The core pathological feature of Parkinson's disease is the loss of dopamine neurons in the substantia nigra. Therefore, directed differentiation of iNSC must focus on the generation of dopaminergic neurons. To achieve this goal, the research team used a specific combination of chemical signals and growth factors to guide the differentiation of iNSC into dopaminergic neural precursor cells. The differentiated cells are not only similar in shape to normal dopaminergic neurons, but also have specific neurotransmitter secretion functions, laying the foundation for achieving alternative functions in the brain after transplantation.
iNSC transplantation and brain target location
The successfully prepared dopaminergic neural precursor cells will then be transplanted into the patient's brain through precise surgical procedures. The key to transplantation surgery is target location to ensure that cells are transplanted into the pathologically affected areas of patients with Parkinson's disease, so as to achieve maximum symptom improvement. To this end, the surgical team used advanced image navigation equipment such as magnetic resonance imaging (MRI) and electroencephalography to inject micro-amounts of cells into the target area after positioning. This process is not only highly precise, but also minimizes damage to surrounding nerve tissue.
Survival and integration of cells after transplantation
After successful iNSC transplantation, these neural precursor cells need to survive, expand and integrate with the host neural network in the patient. The research team found that the transplanted dopaminergic neural precursor cells can survive smoothly in patients with Parkinson's disease, and gradually establish functional connections with the patient's brain tissue to achieve partial recovery of dopamine secretion. During 12 months of follow-up observation, the transplanted cells not only remained active, but also showed high stability.
Discussion on the long-term effect of cell replacement and functional recovery
A potential advantage of iNSC therapy is that the transplanted cells originate from the patient itself and the risk of immune rejection is low. At the same time, this treatment path replaces traditional drug therapy with "cell replacement", allowing patients to achieve longer-term and stable symptom relief. Although the technology is still in clinical trials, the research team expects that the efficacy of iNSC will be further verified as more patients participate in the trial and long-term follow-up data accumulates.
Xuanwu Hospital's world's first iNSC-DAP autologous cell transplantation successfully for Parkinson's disease
The team of Professor Chen Zhiguo from the Cell Therapy Center of Xuanwu Hospital, the team of Professor Zhao Guoguang from the Neurosurgery Department, the team of Professor Chen Biao from the Department of Neurology, the team of Professor Lu Jie from the Department of Radiology and Nuclear Medicine, the leaders of relevant auxiliary departments of the project, and the clinic-level cell preparation company Beijing Huixin Medical Valley Biotechnology Co., Ltd.(hereinafter referred to as Huixin Medical Valley) jointly conducted an in-depth evaluation and discussion on the efficacy.

Ma Jinghong, deputy chief physician of the Department of Neurology of Xuanwu Hospital, introduced in detail the research background, overall design, specific process of the clinical study, and the patient's functional assessment and imaging analysis in the one year since receiving cell therapy.
In the past one year after surgery, the patient's daily prescription time was prolonged, and his later symptoms were significantly improved compared with before surgery. The patient could not stand alone during the preoperative observation period and could hardly take care of himself. In the later period after surgery, the patient could stand and walk alone, and his posture stability was significantly improved, and the overall quality of life was significantly improved. Quantitative comparison of PETMR functional nuclei showed that the standard uptake value (SUVR) on the treated side (right) increased compared with pre-operation, most significantly in the putamen near the graft site.
Results of autologous induced pluripotent neural stem cells in the treatment of Parkinson's disease
It was confirmed that after receiving iNSCDAP treatment, the transplanted dopaminergic nerve cells survived and released neurotransmitters, repairing neural function. All experts agree with the significant efficacy of iNSCDAP after treatment. At the same time, MR imaging scanning showed that no abnormal tissue density was found in the injection area and surrounding brain tissues, and the patient did not experience any serious adverse reactions after surgery, confirming the safety of this treatment method.

Professor Zhao Guoguang commented that this project reflects Xuanwu Hospital's scientific research and medical innovation capabilities and is the result of multidisciplinary collaboration. He hopes that this cell therapy technology can be formed into a product and promoted after receiving more clinical data support to benefit the majority of Parkinson's disease patients.
Professor Chen Biao evaluated that the patient had been closely followed for more than 2 years before transplantation, which provided evidence for longitudinal comparison of efficacy after transplantation and could more fully demonstrate the effect of cell transplantation. Transplantation and evaluation of more enrolled patients will be accelerated in the future.
Advantages and significance of autologous induced neural stem cells in the treatment of Parkinson's disease
iNSC has similar biological properties to neural stem cells in early development and is able to self-renew and differentiate into neurons and glial cells. The cells do not need to go through the iPSC stage, which greatly reduces the risk of tumor formation and improves the safety of transplantation. At the same time, the induction differentiation cycle is shorter, making it an ideal industrial-usable seed stem cell. Not only that, iNSC and other types of neural precursor cells obtained using this technology are also being developed simultaneously, and can also provide new treatment methods and strategies for other nervous system diseases other than Parkinson's disease. This platform technology is an important achievement of China scientists in overcoming the underlying key technologies of stem cell therapy.
The follow-up project team will strictly follow the research plan and work together to jointly promote the smooth implementation of follow-up research, improve the Parkinson's disease cell treatment system, and benefit more Parkinson's disease patients.
Science and Technology innovation
The success of Xuanwu Hospital's iNSC in treating Parkinson's disease marks a major breakthrough in the field of stem cell therapy. Autologous induced neural stem cell technology (iNSC) has several significant advantages over traditional stem cell therapies:
Use of autologous cells with low risk of immune rejection
One of the most significant advantages is that iNSC therapy uses the patient's own cells, which greatly reduces the risk of immune rejection after transplantation. Compared with allogeneic stem cells, autologous cells are more immune receptive and do not require long-term use of immunosuppressants, thereby reducing side effects and treatment costs.
Innovation in transformation technology
By inducing and transforming peripheral blood monocytes into neural stem cells, the Xuanwu Hospital team broke through the limitations of traditional stem cell sources. This technology allows Parkinson's patients to obtain large amounts of neural stem cells through simple blood collection without complex surgery or ethical controversy. Compared with traditional embryonic stem cells, iNSC technology is more mature and ethically acceptable.
Efficient targeted differentiation and brain-targeted therapy
iNSC technology not only solves the problem of cell origin, but also enables these stem cells to effectively differentiate into dopaminergic neurons in patients through efficient directed differentiation technology. This provides new ideas for the fundamental treatment of Parkinson's disease, which is to repair damaged areas through cell replacement rather than simple drug treatment or nerve stimulation. The proposal of this idea has brought the treatment of neurodegenerative diseases into a new era.
future prospects
With the continuous optimization of iNSC technology and the accumulation of clinical data, it is expected that its application will be widely promoted in the next few years, not only limited to Parkinson's disease, but also extended to the treatment of other nervous system diseases. In addition, with the development of gene editing technology, future iNSC treatments will be more personalized and precise, providing patients with more efficient and safer treatment options.