
Have you ever thought about how human organs develop step by step? What happens when they get sick? To answer these questions, scientists turned their attention to a magical small laboratory product-organoids. Although these miniature organs are only a few millimeters in size, they are carefully constructed by cells in a culture dish and can imitate the function and structure of real organs.
Recently, in a research report published in the international journal Nature Cell Biology titled "Blood-generating heart-forming organics recapitulate co-development of the human hematopoietic system and the embryonic heart", researchers from institutions such as the Hanover Medical School in Germany successfully developed the first blood-generating heart-forming organism (BG-HFO) that can produce blood. This research not only provides a new perspective on understanding the co-development of the heart and blood systems, but may also open the way for future treatment of multiple diseases.

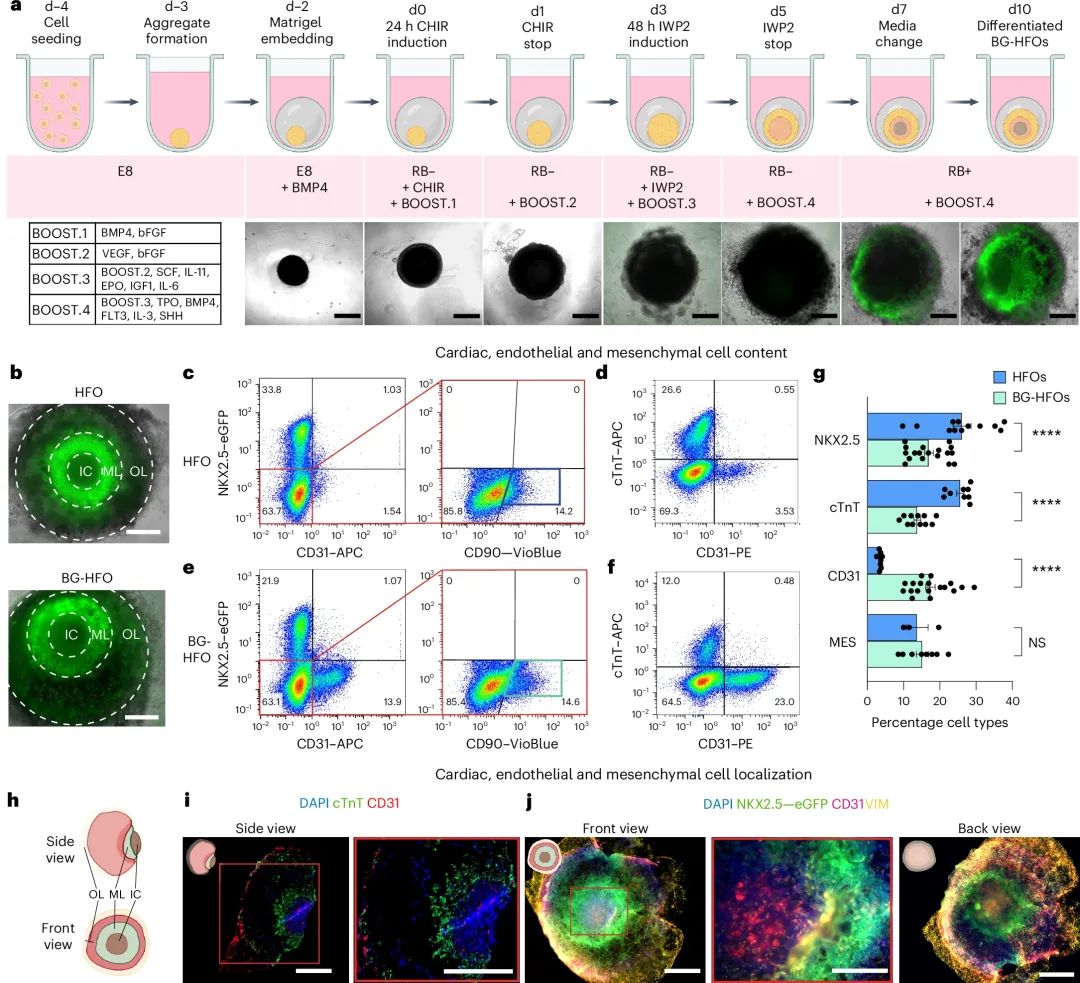
Imagine if you could hold a small, embryo-like heart under a microscope and observe it, what would you see? Using this organoid model, the researchers recreated the coordinated development of the heart and blood system in three-dimensional space. This is like observing the origin and development of life in a small universe. Creating such organoids is not easy, requiring precise timing and a complex series of steps, including the addition of specific nutrients, growth factors and signaling molecules. These ingredients must be added in a strict order, just like cooking an exquisite meal, where every step is crucial.
As early as 2021, researchers have successfully created heart-forming organoids (HFO) for the first time, which can reproduce the entire process of early development of the human heart in cell culture.
However, only now have they solved the problem of combining simulated heart development and hematopoietic processes. Because blood production in human embryos begins around the fourth week, near the aorta, this time and location are very close to the heart blood vessels. Based on previous cardiac organoid models, the researchers gradually added special factors to create a new type of BG-HFO. These organoids are made from human pluripotent stem cells (hPSC), which have the ability to reproduce indefinitely and differentiate into any type of cell.
 BG-HFOs或能展现出心脏、内皮和间质的组分
BG-HFOs或能展现出心脏、内皮和间质的组分
With the help of a hydrogel matrix, the researchers cleverly controlled hPSCs so that they developed into heart organoids within 10 to 14 days. These artificial hearts are not just a simple collection of cardiomyocytes, but complex structures made up of at least seven different cell and tissue types, similar to the three cup-shaped layers in natural embryos, including the heart's mesenchymal prima (anlagen), precursors of the liver and lungs, and blood vessels. As Dr. Miriana Dardano explains,"We have adjusted the differentiation steps and added a dense endodermis to the heart organoid, an endothelial layer that lines the blood vessels and from which blood-forming cells and progenitor cells emerge."
The significance of this research is not only its technological breakthrough, but more importantly, it provides a platform for other researchers to study cross-tissue interactions in the hematopoietic process in cell culture. These findings are crucial to understanding the development and blood-making processes of healthy organs.
In addition, BG-HFO can also serve as a model for diseases such as COVID-19, helping scientists better understand and treat cardiovascular diseases. After all, diseases like COVID-19 can attack the heart, blood vessels and even lungs, and organoid models may more accurately reflect the human response than animal models, because the latter are influenced by other biological factors and the results can only be limited. To humans.
Looking to the future, researchers do not stop at the heart and blood. They have begun exploring a new differentiation method to transform hPSC starter cells into cells from other organs, thereby building organoid models containing multiple tissues for medical research. This is like having a flexible set of construction tools that can build different types of "mini organs" as needed, opening the door for future medical innovation.