
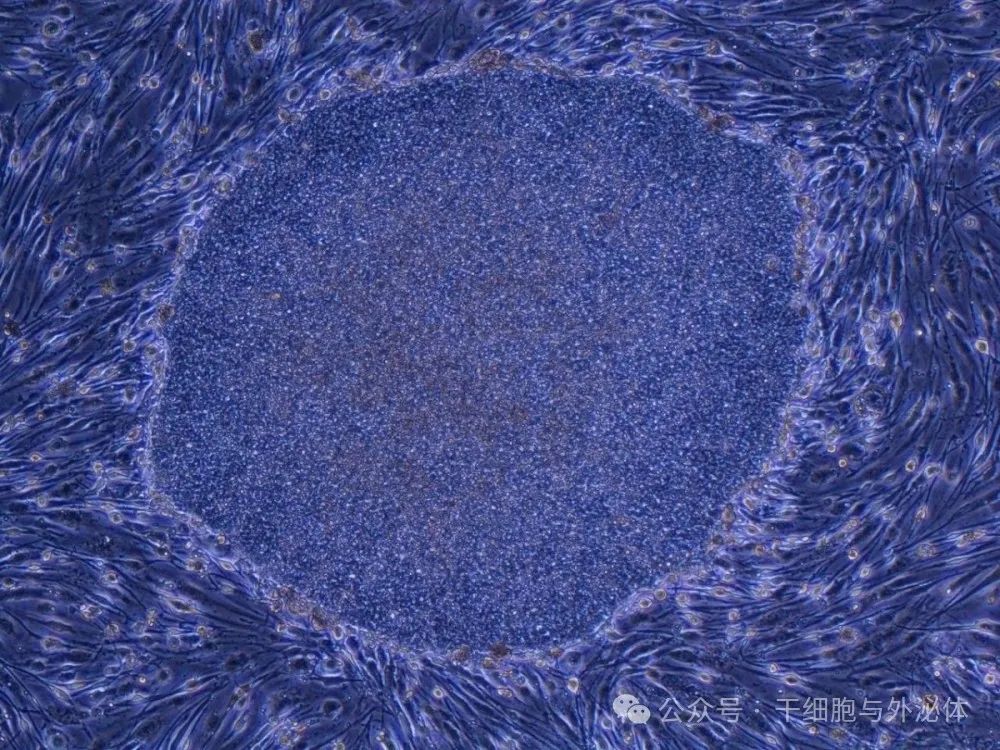
Figure: A human induced pluripotent stem cell (iPS) community established from fibroblasts. Kyoto University Hospital is seeking to use iPS cells to treat type 1 diabetes.
The hospital announced on September 5 that it will start clinical trials as early as February next year and transplant such islet cell cells into three patients. If proven safe and effective, the study could pave the way for a treatment that would allow people with type 1 diabetes to take daily insulin injections. Currently, 100,000 to 140,000 people in Japan suffer from the disease.
After clinical trials, the researchers hope to achieve approval for marketing using iPS cell-derived islet cell transplantation to treat type 1 diabetes within five years.
In the trial, the researchers transplanted the pancreatic cells into three patients with severe type 1 diabetes. The patients, aged between 20 and 65 years, will also receive immunosuppressants and insulin treatment during the trial.
The researchers will use islet cells derived from human induced pluripotent stem cells (iPS cells), developed by Taro Toyoda, a researcher at the Kyoto University Center for iPS Cell Research and Applications (CiRA). Shinya Yamanaka, founding director of CiRA, won the Nobel Prize in Physiology or Medicine in 2012 for the discovery of iPS cells, mature cells that can be reprogrammed into any type of cell.
In clinical trials, iPS cells from healthy donors will be transformed into islet cells, laid on a thin sheet, and transplanted into patients. For one year after transplantation, researchers will closely monitor the patient's condition to check for adverse side effects.
The pancreas of people with type 1 diabetes produces almost no insulin. As a result, they need regular injections of insulin, a hormone that converts glucose into energy. The exact cause of type 1 diabetes is unclear, but it occurs when the body's immune system destroys the islets of insulin in the pancreas.
In Japan, pancreatic cell transplants from deceased people have been approved for public health insurance, but few patients receive such transplants due to a shortage of donors.
Daisuke Yabe, a diabetes expert at Kyoto University who led the project, said: "We would be very happy if we could see a world where insulin injections were no longer needed. We hope this will be the first step towards fundamentally curing this disease."
Relevant research progress in my country
People with type 1 diabetes usually require abdominal injections of insulin products multiple times a day. When you have type 1 diabetes, the so-called islet cells in the pancreas that produce insulin are dysfunctional and cannot control the patient's blood sugar levels. There are an estimated 100,000 to 140,000 people with type 1 diabetes in Japan.
In January 2023, the research team of Deng Hongkui of Peking University and the research team of Peng Xiaozhong of the Chinese Academy of Medical Sciences/Peking Union Medical College collaborated to publish a research paper titled "Implantation underlying the abdominal anterior rectus sheath enables effective and functional implantation of stem cell-derived islets in Nature Metabolism." This research developed a new islet transplantation strategy that effectively supports the survival, functional maturity and long-term maintenance of functions of pancreatic cells differentiated from human induced pluripotent stem cells.
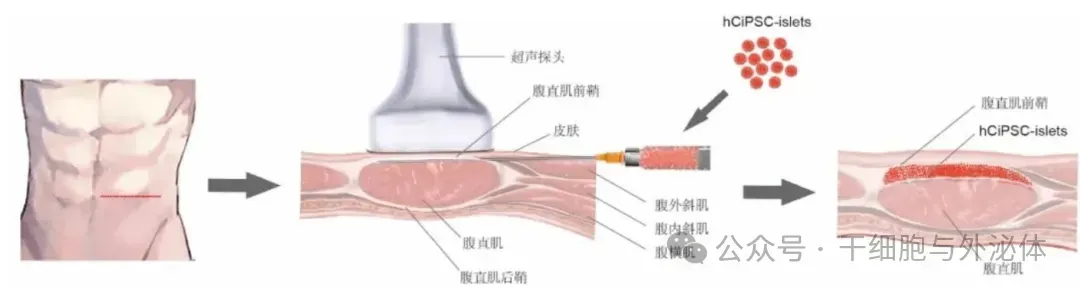
Figure: Schematic diagram of transplantation of islet cells into the anterior sheath of the rectus abdominis muscle derived from human induced pluripotent stem cells.
On July 11, 2023, Peking University released a piece of heavy news about diabetes treatment: Peking University Stem Cell Research Center cooperated with Tianjin City First Central Hospital to successfully complete the world's first islet cell transplant operation for chemically reprogramming iPS cell differentiation in a subject with type 1 diabetes. This treatment technology is expected to become an ideal solution to completely cure type 1 diabetes.