
Source:eMedClub
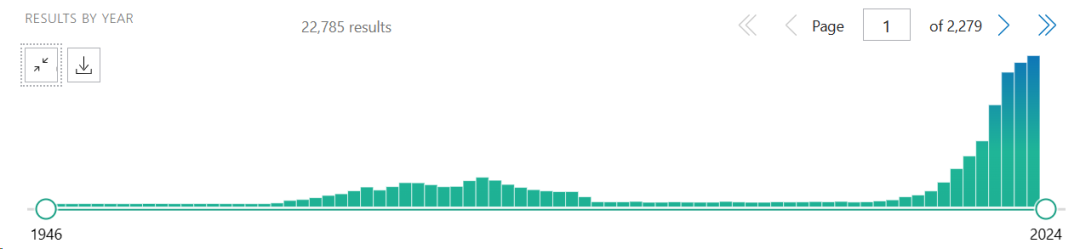
Compared with traditional 2D cell culture models, Organoids can better simulate physiological and pathological states and the occurrence process of organs and tissues, making up for the limitations of existing models, and have been widely used in cancer research, disease modeling, drug screening, regenerative medicine, precision medicine and other fields. According to PubMed data, in recent years, organoids related research has shown an increasing trend year by year, becoming a hot frontier track.
An article has reported the use of cartilage organoids derived from allogeneic induced pluripotent stem cells (iPSC) in the treatment of articular cartilage defects. The researchers used iPSC to generate cartilage composed of chondrocytes and extracellular matrix (ECM), and transferred it to a three-dimensional culture for further cultivation so that the derived cartilage produces ECM and accumulates around it to form cartilage tissue particles. In theory, due to the self-renewal activity of iPSC, cartilage tissue derived from allogeneic iPSC can be produced indefinitely and transplanted into an unlimited number of patients to solve the problems of donor shortage, disease transmission, and quality differences, but it is still difficult to achieve.
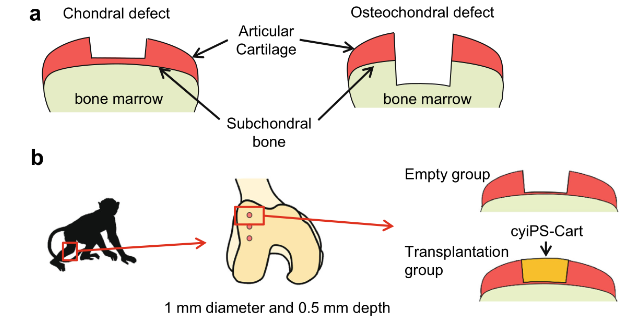
▲ Primate animal organoid transplantation
At the time of publication, no studies had evaluated allograft cartilage into primate models, and this study analyzed in depth the allograft of IPSC-derived cartilage organoids without the use of immunosuppressive drugs. The results showed that allogeneic IPSC-derived cartilage organoids survived, integrated, and remodeled into articular cartilage in primate models of knee cartilage defects without eliciting an immune response and contributing to tissue repair for at least 4 months. The transplanted cartilage organoids integrate with the host's natural articular cartilage and prevent degradation of the surrounding cartilage. Single-cell RNA sequencing and molecular biological analysis of the grafts showed that SIK3, PRG4 and cell differentiation-related pathways were involved in the remodeling and repair of cartilage after transplantation.
The results of this study suggest that allotransplantation of IPSC-derived cartilage organoids may be clinically suitable for the treatment of articular cartilage defects.
The therapeutic potential of organoid transplantation is emerging
Research into organoids being used for transplantation into other living organisms to assess regenerative capacity has paved the way for the use of organoids in regenerative medicine. Compared with implantable medical devices, organoids have the advantages of more functional diversity, less rejection, less susceptibility to magnetic fields or physical influences, and can also be genetically corrected in the case of genetic abnormalities by replacing damaged organs with recovered tissue. At present, many studies have reported the application potential of organoids in regenerative medicine/organ transplantation.
Recently, an article in Cell Stem Cell reported that researchers from Cincinnati Children's Hospital in the United States cultured human colon organoids (Hcos) derived from pluripotent stem cells, developed hematopoietic endothelium-like cells and related RUNX1+ cells, red bone marrow progenitor cells, and eventually produced functional resident macrophages. After transplantation into mice, HCO macrophages remain within colonic organoids and are not replaced by host bone marrow-derived macrophages. The project paves the way for research into producing human organoids containing resident immune cells.
In July last year, a research team at Tokyo Medical and Dental University in Japan carried out the first clinical study of stem cell-derived organoids transplanted into humans, and they transplanted organoids grown from the patient's own healthy intestinal mucosal stem cells into a patient with refractory ulcerative colitis. The organoids are transplanted into patients with the large intestine, then covered with a membrane that degrades in the human body and fixed using the patient's own tissue to repair the mucosa. The patient is in good condition after treatment.
Previously, in a study published in Science, researchers grew a bile duct-like organoid and transplanted it into mice with chemical damage to the bile ducts. It was able to fuse with host cells and regenerate damaged tissue, significantly extending the survival of mice compared to controls. The researchers then grew new human organ tissue and transplanted it in vitro into three donor human livers. These organoids were able to repair damaged bile ducts and restore their function, allowing the organs to be transplanted into patients. This brings new options for liver treatment and new feasible ideas for repairing donated organs.
An article in Nature Biomedical Engineering reported that Zhicheng Shao's team at Fudan University developed a method to induce astrocytes to become neuroorganoids (Op53-CSBRY). After the resulting spinal cord organoids with the function of dorsal and ventral neurons of the spinal cord were transplanted into mice, the organoids survived and differentiated into spinal neurons. And form synapses with host neurons, improving motor function in mice.
Sum up
Organoids have been proved in many studies to have strong transplantation repair ability and good safety. There are many researches in the fields of intestine, liver, heart, etc. However, due to the complexity of organoids, there are high requirements on culture system, vascular system, engineering, etc. Most of them are still in the early stage of research, and there is still a long way to go to achieve clinical transformation. In the future, with the development of organoid technology, perhaps the field of organ transplantation/regenerative medicine will usher in major progress.