
On October 7, 2024,"Analysis of the National Burden and Risk Factors of Diabetes in China from 1990 to 2021: Results of the Global Disease Burden Study in 2021" was released in the Journal of Diabetes.
The analysis of the report shows that in the more than 30 years from 1990 to 2021, the age-standardized incidence, prevalence and disability-adjusted life years (DALYs) of overall diabetes, type 1 diabetes and type 2 diabetes in my country showed an overall growth trend, and the mortality rate of diabetes showed a downward trend. Middle-aged and elderly men face a greater disease burden.
01 Diabetes

Type 2 diabetes is the main burden of diabetes in my country.
In 2021, the number of people suffering from diabetes in my country will exceed 4 million, the total number of people suffering will exceed 117 million, and the number of deaths will exceed 178,000.
The age-standardized incidence, prevalence and disability-adjusted life years (DALYs) of diabetes have generally increased over the past three decades, and can be attributed to improvements in economic and social development, extended survival from chronic diseases such as hypertension and hyperlipidemia, and unhealthy lifestyles, including factors such as smoking, alcohol consumption and prolonged sedentary behavior.
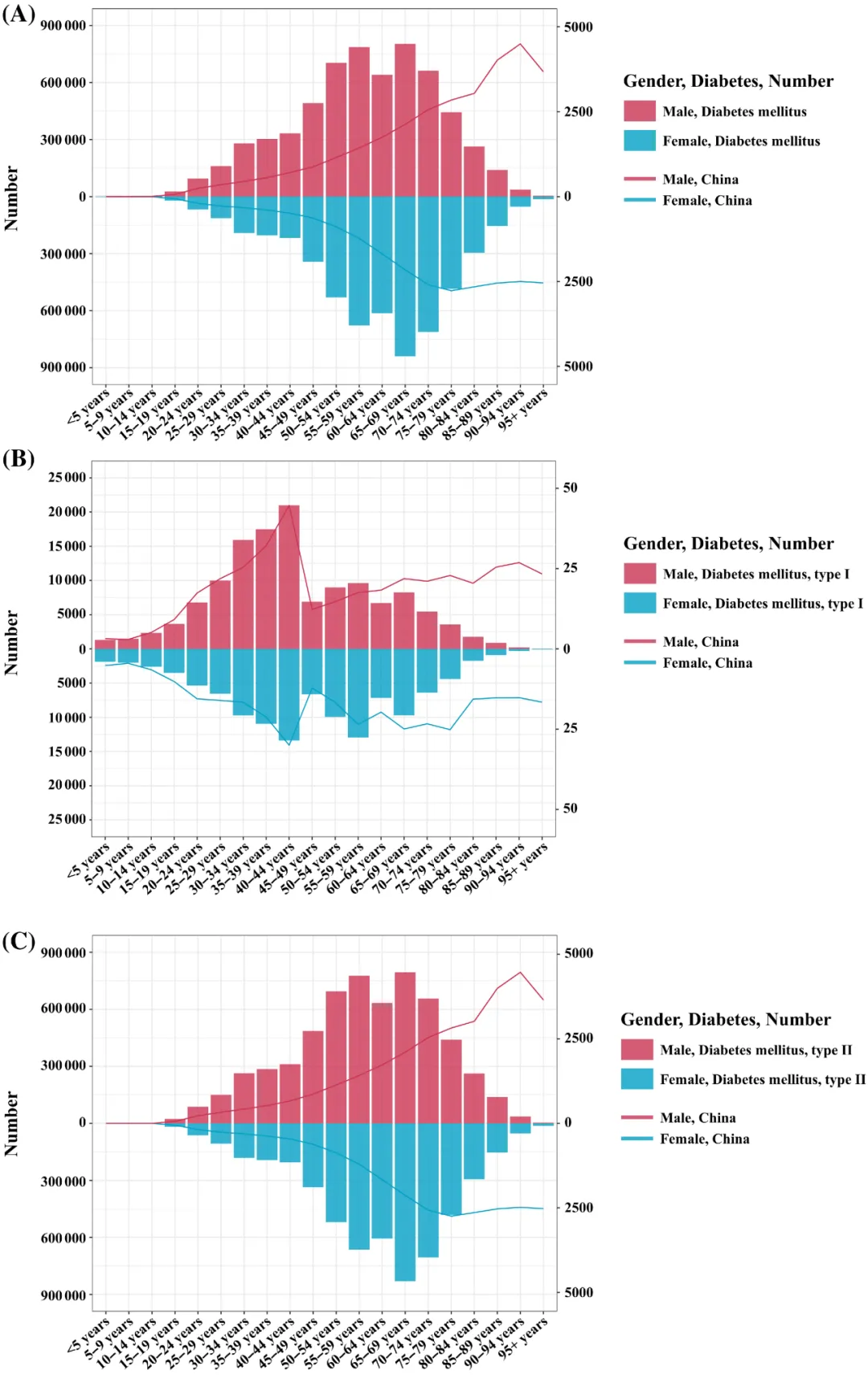
Absolute value and age-standardized DALYs for men and women by age group in China in 2021 (per 100,000 person-years)
Notes: (A) Diabetes;(B) Type 1 Diabetes;(C) Type 2 Diabetes
In addition, population aging is an important driver of the increase in the incidence and prevalence of diabetes. However, the age-standardized death rate of diabetes is on a downward trend, indicating that the risk of diabetes-related death in my country has decreased, which may be related to the improvement of medical services and progress in medical care in recent years.
Severe complications caused by diabetes can affect multiple organ systems, including the heart, blood vessels, eyes, kidneys and nerves. These complications not only affect the patient's quality of life, but also significantly increase the cost of treatment. According to studies, the cost of treatment for diabetic patients with complications is significantly higher than for patients without complications. However, in China, the awareness rate of diabetes is only 36.5%, the treatment rate is 32.2%, and the treatment rate is only 49.2%.
In terms of diabetes types, type 2 diabetes is the main burden of diabetes in China, mainly occurring in adulthood, and obesity is an important risk factor.
From a gender perspective, in most age group analyses between 1990 and 2021, men in my country have higher disability-adjusted life years (DALYs) than women. This difference may be related to men's exposure to obesity, smoking, excessive drinking, and sedentary behavior. A higher degree of risk factors such as behavior.
In terms of age distribution, the high incidence of disability-adjusted life years (DALYs) caused by overall diabetes and type 2 diabetes in China in 2021 will be between the ages of 50 and 74. The value and ratio of DALYs continue to increase with age, peaking in the 65-69 age group, indicating that diabetes has a greater impact on the elderly. For type 1 diabetes, the peak in DALYs occurs in middle age, especially among adults aged 40-44.
Analysis of diabetes risk factors shows that multiple risk factors have a significant impact on diabetic DALYs in my country, including high fasting blood sugar, high BMI, dietary risks, air pollution, tobacco, low physical activity, inappropriate temperature and alcohol consumption.
Among them, diabetes-related DALYs caused by high fasting blood sugar remain at a high level. DALYs caused by dietary risks, alcohol consumption and high BMI increased, while DALYs caused by air pollution, tobacco, low physical activity and inappropriate temperature decreased.
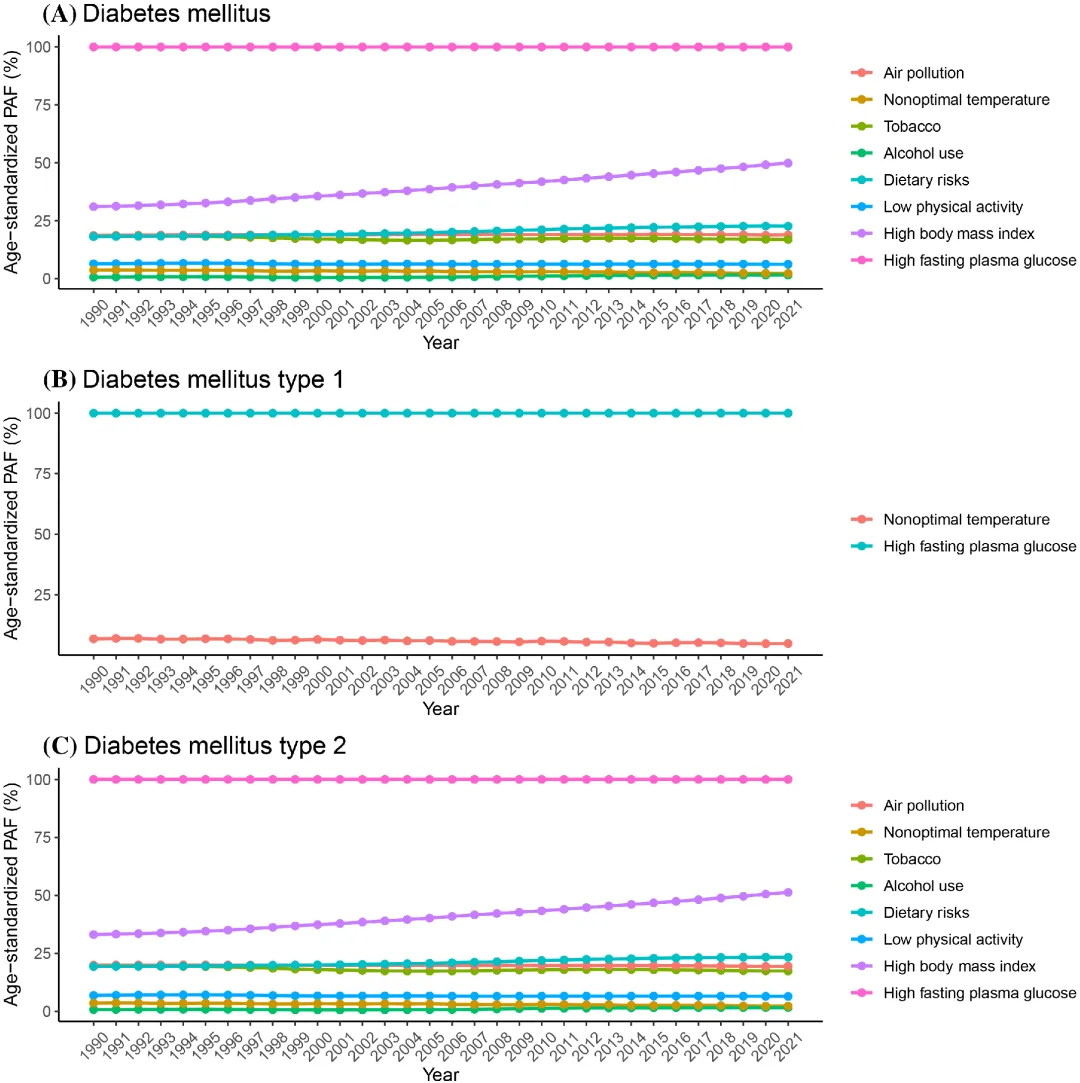
Age-standardized population attribution scores (PAF) for disability-adjusted life years (DALYs) due to risk factors in China between 1990 and 2021.
(A)Diabetes;(B) Type 1 diabetes;(C) Type 2 diabetes.
02 Diabetes stem cell therapy

Multiple clinical studies have confirmed the efficacy and potential of stem cell therapy in the field of diabetes.
In recent years, more and more studies have confirmed the effectiveness and safety of stem cell therapy in the treatment of diabetes, bringing new hope and choices to diabetic patients!
Mesenchymal stem cells (MSCs)
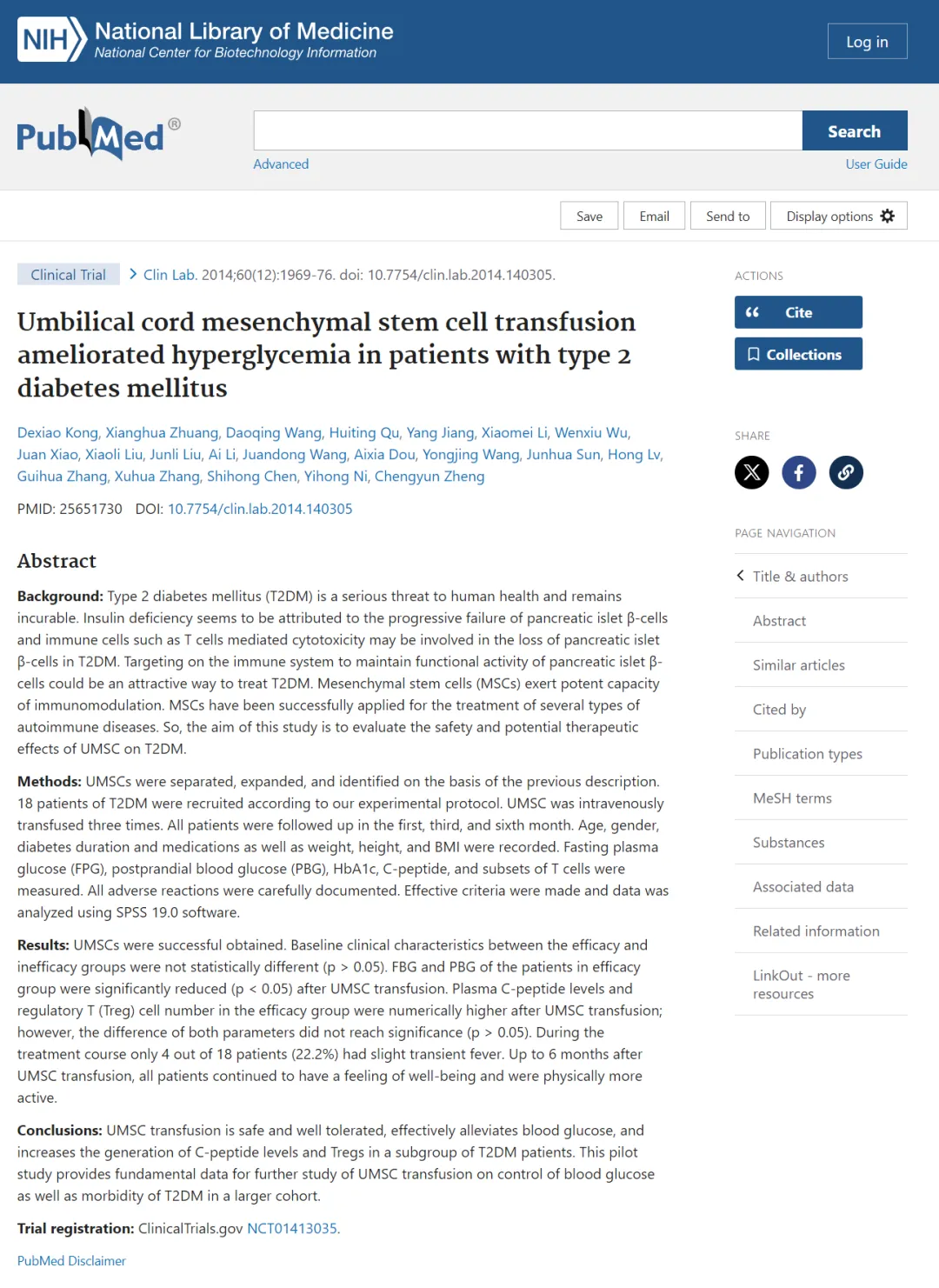
Clinical trials of umbilical cord derived mesenchymal stem cells (UC-MSCs) transplantation for the treatment of type 2 diabetes are mainly divided into self-control and placebo-control, focusing on their efficacy and safety.
Current clinical trials generally study the efficacy of UC-MSCs transplantation alone, but there is little progress in clinical research on its combination treatment with other drugs.
1. Can improve hyperglycemia in patients with type 2 diabetes
A research team from the Second Hospital of Shandong University in China published a clinical observation report titled Umbilical cord mesenchymalstem cell fusion ameliorated hyperglycemia in patients withtype2 diabetes mellitus in the journal Clin Lab, demonstrating that umbilical cord mesenchymal stem cell (UC-MSCs) infusion can improve hyperglycemia in patients with type 2 diabetes mellitus (T2DM).
In this project, the researchers selected 18 patients with T2DM aged 23 to 65, who were infused with UC-MSCs(1 x 10/kg) three consecutive intravenous infusions and were followed up for 6 months. After 6 months, they found that 8 patients had post-transplantation. The demand for antidiabetic drugs or insulin was reduced by more than 1/3 or the blood sugar level was reduced by more than 20%, and the 2-hour C-peptide level and T cell percentage were significantly increased compared with before the experiment, indicating that their pancreatic β cell function was improved.
2. Glycosylated hemoglobin decreased significantly
China scholars published clinical observation results titled A preliminary evaluation of effi-cacy and safety of Wharton's jelly mesenchymal stem cell trans-planting in patients with type 2 diabetes mellitus in the journal Stem CellRes Ther, demonstrating the efficacy and safety of umbilical cord mesenchymal stem cell (UC-MSCs) transplantation in the treatment of type 2 diabetes mellitus (T2DM).
In this project, the researchers treated 22 patients with T2DM through intravenous infusion of UC-MSCs and conducted a 12-month self-control study. The results showed that the average glycosylated hemoglobin (HbAlc) monitored at 1, 3, and 6 months was significantly lower than before treatment, and stabilized at the end of the treatment.(7.00%±0.60%), which remained at a low level during the follow-up period; the C-peptide level peaked at (1.95±1.30)ng/ml at the sixth month, and fell slightly in the subsequent period; After receiving UC-MSCs transplantation, the injection dose of patients who needed insulin injection was significantly reduced, and one patient who originally needed oral antidiabetic drugs could discontinue antidiabetic drugs after receiving transplantation.

3. High insulin demand has significant improvement
The research team of the First Medical Center (301 Hospital) of the General Hospital of China People's Liberation Army published a report titled Effectiveness and safety of umbilical cord-derived mesenchymal stem cells in Chinese adults with type 2 diabettes in the journal Stem Cell Res Ther in 2022: The clinical observation results of a single-center, double-blinded, randomized, placebo-con-rolled phase II trial demonstrate that umbilical cord mesenchymal stem cell (UC-MSCs) transplantation may become a potential treatment for adult type 2 diabetes (T2DM) patients in China.
The researchers conducted a 48-week single-center, randomized, double-blind, placebo-controlled phase 2 clinical study in which 91 patients were randomly assigned to the UC-MSCs group [n=45, 100 ml of UC-MSCs were infused intravenously (1×10^6 cells/kg)] versus placebo group (n=46, intravenous infusion of a solution consisting of equal amounts of NS, 3% human albumin and 0.5ml of vitamin complex), the treatment frequency was once every 4 weeks, and the infusion was 3 times in total; after 48 weeks, the HbA1c content in the UC-MSCs group was significantly reduced compared with before treatment, and the daily insulin demand decreased more significantly, which suggests that UC-MSCs transplantation has a significant improvement effect on hyperglycemia and high insulin demand in patients with T2DM.

Induced pluripotent stem cells (iPSC)
Induced pluripotent stem cells (iPSC) have shown great potential in the treatment of diabetes. They not only can differentiate into insulin-producing cells to replace damaged islet cells, but also have significant advantages in personalized medicine. iPSC technology allows cells to be extracted from a patient's own tissue, reprogrammed into stem cells, and redifferentiated into the desired cell type, thereby reducing the risk of immune rejection. In addition, iPSC also plays an important role in the creation of disease models, which can simulate the pathological process of diabetes and provide an important tool for studying disease mechanisms and testing new treatments.
1. The world's first! Chemically reprogrammed induced pluripotent stem cells treat type 1 diabetes to achieve functional cure
On September 25, 2024, the research teams of Shen Zhongyang and Wang Shusen of Tianjin City First Central Hospital and Deng Hongkui's team of Peking University/Changping Laboratory published an article in "Cell" titled Transplantation of chemically induced pluripotent stem-cell-derived islets under abdominal anterior rectus sheath in a type 1 diabetes patient. For the first time in the world, type 1 diabetes has been clinically functionally cured through innovative stem cell islet transplantation. The patient no longer required exogenous insulin treatment during the 1-year follow-up period.
The principle of this transplantation method is based on the fact that iPSC has unlimited proliferation characteristics and can differentiate into all functional cell types in the organism. Professor Deng Hongkui, the developer of this technology, just won the Future Science Award known as the "China Nobel Prize" in August this year. His contribution is to "creating 'Chemically Induced Pluripotent Stem Cells'(CiPSC)" and changing the fate and state of cells. Outstanding achievements."
2. The world's first! Stem cell regenerative islet transplantation, 25-year history of diabetes cured patient
On April 30, 2024, Professor Yin Hao's team from the Second Affiliated Hospital of Naval Medical University (Shanghai Changzheng Hospital), together with Professor Cheng Xin's team from the Center for Excellence and Innovation in Molecular Cell Science, China Academy of Sciences, published a research result entitled Treating a type 2 diabetic patient with implanted pancreatic islet function by personalized endoderm stem cell-derived islet tissue on Cell Discovery. This is the first time in the world that autologous regenerative islet transplantation derived from induced pluripotent stem cells (iPS cells/iPSC) has been successfully used to successfully cure diabetes with severely impaired islet function.
The patient was a 59-year-old male with a 25-year history of T2DM and developed end-stage diabetic nephropathy (uremia). In June 2017, he developed end-stage diabetic nephropathy and received a kidney transplant. On July 19, 2021, due to concerns about hypoglycemia and considering the adverse impact of poor blood sugar control on the long-term survival of the donor kidney, the patient received autologous regenerative islet transplantation at Shanghai Changzheng Hospital. It is worth noting that insulin needs were gradually reduced until the drug was completely discontinued at the end of week 11, and oral antidiabetic drugs were gradually reduced starting from week 44 and discontinued at weeks 48 and 56.
After decades of exploration and testing, stem cell therapy is leading the medical community through a major revolution. In the field of diabetes treatment, the use of stem cells has had a profound impact. As scientific research continues to deepen, mankind is becoming increasingly hopeful on the road to overcoming the long-term challenge of diabetes. Stem cell-based diabetes replacement therapies have not only shown strong feasibility, but also opened up broad potential application prospects, bringing patients a promising new treatment option.